The Thyroid and Testosterone Connection Explained
Your thyroid and testosterone are locked in a powerful, direct relationship—a problem with one almost always spells trouble for the other. Think of your body’s endocrine system as a finely tuned orchestra. In this orchestra, your thyroid and your testosterone production are two lead instruments that must play in perfect harmony. If your thyroid starts playing too fast or too slow, it throws the entire hormonal symphony out of whack, dragging testosterone down with it.
This is the root cause of symptoms that so many men struggle with, like persistent fatigue, brain fog, and a libido that’s gone missing.
The Hormonal Feedback Loop: Thyroid and Testosterone
This guide dives into the critical, and frankly, often-overlooked link between these two hormonal powerhouses. It’s incredibly common for men to chase symptoms, trying to fix low energy or a lagging sex drive without ever realizing their thyroid is the real problem. Getting a handle on this connection is the first real step toward genuine optimization.
Ignoring this interplay is also one of the biggest reasons why treatments like Testosterone Replacement Therapy (TRT) sometimes fail to deliver the results you expect. If an underlying thyroid issue is the true culprit behind your low T symptoms, starting TRT without fixing it first is like trying to solve an engine knock by getting a new paint job—it completely misses the point.
It’s a Two-Way Street
This isn't just a one-way street where the thyroid dictates all the terms. The communication flows in both directions, creating a sensitive feedback loop that your body relies on to maintain a delicate hormonal balance. For men dealing with low testosterone (hypogonadism), this interaction is especially crucial.
Research has shown that testosterone directly influences thyroid hormone production. It can actually boost levels of T4 (the inactive thyroid hormone) while simultaneously lowering TSH, which is the pituitary gland's signal to kick the thyroid into gear. This effect is most noticeable in men who start with low testosterone, suggesting that restoring T levels can, in turn, help optimize thyroid output. For a deeper dive into this dynamic, you can explore the relationship between thyroid and testosterone levels.
Think of it like this: Your thyroid sets the metabolic pace for your entire body. When it’s underactive, every system slows to a crawl, including the intricate machinery responsible for making testosterone. On the flip side, an overactive thyroid can flood your system with proteins that bind up your free testosterone, making it useless.
To really get a handle on your health, you have to look at the complete picture. That means looking beyond single hormone markers and appreciating how the entire endocrine system functions as a team.
Throughout this guide, we'll break down:
- Symptom Overlap: Why it’s so easy to mistake a thyroid problem for low testosterone, and vice versa.
- Essential Lab Work: The specific tests you absolutely need to get a clear and accurate diagnosis.
- Strategic Treatment: Why fixing the thyroid first is often the most effective path to restoring total hormonal health.
By the time we're done, you'll have the knowledge you need to have more informed conversations with your doctor and take back control of your hormonal well-being.
Understanding Your Hormonal Command Center
To really get the connection between your thyroid and testosterone, you first have to appreciate your body’s internal chain of command. Two incredibly powerful systems, working in parallel, dictate a huge part of your energy, mood, and overall vitality. These are the Hypothalamic-Pituitary-Thyroid (HPT) axis and the Hypothalamic-Pituitary-Gonadal (HPG) axis.
Think of the whole operation like a sophisticated corporate headquarters. The hypothalamus, a tiny region at the base of your brain, is the CEO. It’s constantly monitoring your body’s status and issuing top-level directives.
Just below it sits the pituitary gland, acting as the diligent middle manager. This gland takes the CEO's orders and translates them into specific instructions for the "factory floors"—in this case, the thyroid and the testes. This ensures the right messages get to the right departments at precisely the right time.
The Two Key Production Lines
These two axes, while separate, are deeply intertwined and run on similar principles. Understanding how both of them work is the key to figuring out where a breakdown in communication might be sabotaging your hormonal health.
-
The HPT Axis (Thyroid Production): When the CEO (hypothalamus) senses you need more metabolic energy, it sends out a memo called Thyrotropin-Releasing Hormone (TRH) to the manager (pituitary). The pituitary then releases Thyroid-Stimulating Hormone (TSH) into your bloodstream, which tells the thyroid gland to get to work producing its hormones, T4 and T3.
-
The HPG Axis (Testosterone Production): A similar process happens for testosterone. The hypothalamus releases Gonadotropin-Releasing Hormone (GnRH). The pituitary responds by sending out Luteinizing Hormone (LH), which signals the testes to start manufacturing testosterone.
Both of these systems rely on a brilliant bit of engineering: the negative feedback loop. Once the factory floors (thyroid and testes) have produced enough hormones, those hormones travel back up to the brain and tell the CEO and manager to stop sending signals. This elegant process prevents overproduction and keeps the entire system in a state of balance.
This diagram shows how a signal from a gland like the thyroid can ultimately influence how your body feels and functions.
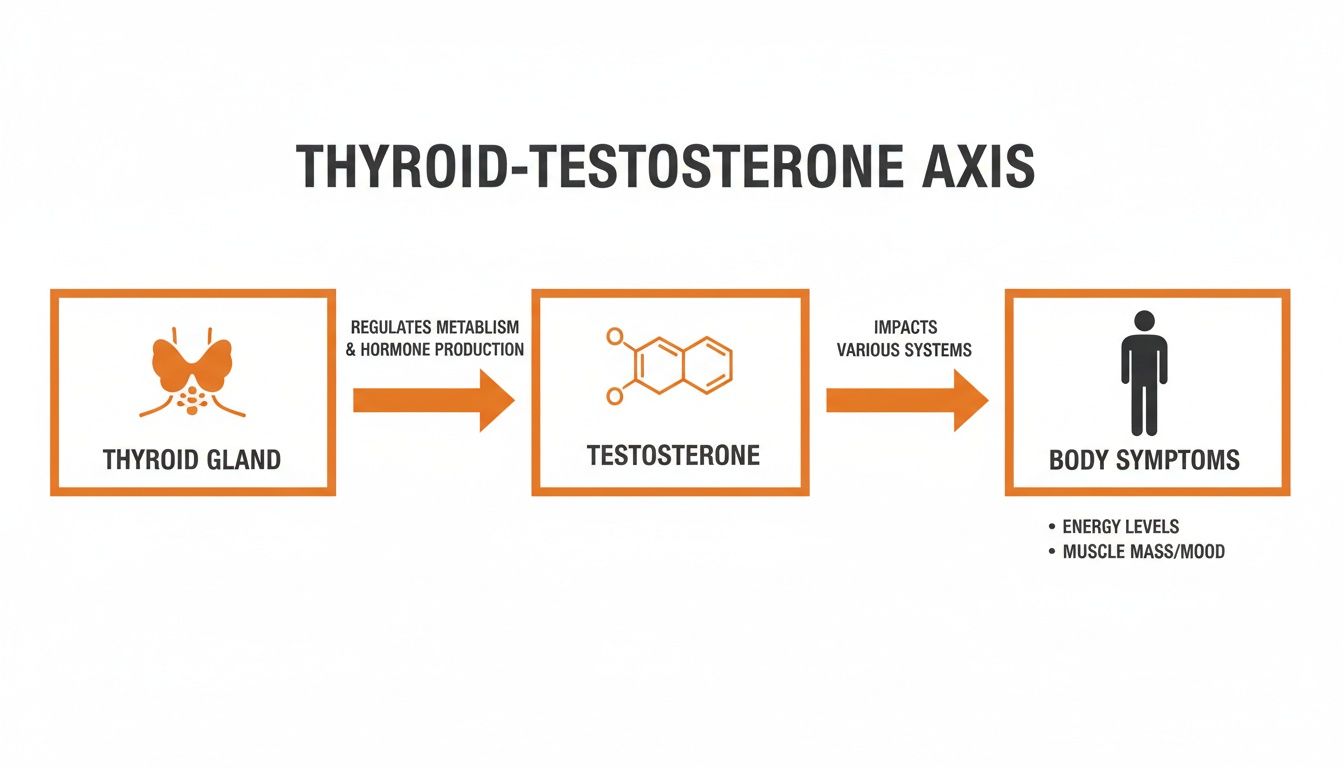
As you can see, there’s a direct pathway from gland to hormone to symptom. An issue right at the source creates noticeable effects all over the body.
Where Communication Breaks Down
So, how do these two seemingly separate departments end up interfering with each other? The connection happens through shared resources and overlapping chemical messengers. Put simply, the efficiency of one axis directly impacts the other.
A key player in this crosstalk is Sex Hormone-Binding Globulin (SHBG), a protein made mostly in the liver. Your thyroid hormone levels have a major influence on how much SHBG your liver pumps out. When thyroid hormones are high (hyperthyroidism), SHBG levels tend to shoot up right along with them.
This is where the trouble starts. SHBG acts like a magnet for testosterone. When SHBG levels are elevated, it binds to testosterone molecules, rendering them inactive and completely unusable by your cells.
This means you could have "normal" total testosterone on a lab report, but if all your free, usable testosterone is tied up by excess SHBG, you'll still experience all the classic symptoms of low T. It’s a perfect example of how an overactive thyroid can directly sabotage your testosterone function, even if your HPG axis is working perfectly.
This foundational knowledge is absolutely critical. It helps you see your endocrine system not as a collection of separate parts, but as one interconnected network where a problem in one area will inevitably cause ripples in another. By understanding this command center, we can get much better at identifying the true source of your symptoms.
How Thyroid Imbalances Sabotage Testosterone Levels
Now that we’ve pulled back the curtain on the hormonal command center, we can get specific about how a glitch in your thyroid’s programming can directly dismantle your testosterone levels. These two systems are so deeply connected that a problem in one almost always creates a cascade of frustrating issues in the other.
A thyroid imbalance typically shows up in one of two ways: hypothyroidism (an underactive thyroid) or hyperthyroidism (an overactive thyroid). Both are bad news for testosterone, but they go about their sabotage in completely different ways.
Hypothyroidism: The System-Wide Slowdown
When your thyroid is underactive, it’s like someone turned down the master thermostat for your entire body. Everything slows to a crawl—your metabolism, your heart rate, and yes, your hormone production. This system-wide deceleration throws a wrench directly into the HPG axis, the system in charge of making testosterone.
The pituitary gland, that diligent middle manager, gets sluggish. It becomes less sensitive to signals and cuts back its output of key hormones. Specifically, it dials down the release of Luteinizing Hormone (LH), which is the direct order telling your testes to produce testosterone. With fewer orders coming from headquarters, the factory floor grinds to a halt, and your T levels plummet.
A sluggish thyroid doesn’t just make you feel tired; it actively mutes the hormonal signals your body needs to synthesize testosterone. Getting the production line running at full capacity again means you have to address the root cause—the hypothyroidism itself.
Hyperthyroidism: The Free Testosterone Paradox
An overactive thyroid is a bit more deceptive and often leads to a confusing clinical picture. A man with hyperthyroidism might get his lab report back and see normal—or even high—total testosterone. This is a classic hormonal paradox that frequently leads to misdiagnosis, leaving the man to suffer with all the debilitating symptoms of low T despite what the numbers say.
The real villain in this scenario is Sex Hormone-Binding Globulin (SHBG). As we've covered, your thyroid hormones directly regulate how much SHBG your liver produces. So, when your thyroid goes into overdrive, it signals the liver to flood your system with a massive amount of SHBG.
Think of SHBG as a sponge. It soaks up testosterone molecules, binding to them so tightly that they become biologically inactive. So while your total testosterone might look fine on paper, the amount of usable free testosterone—the hormone that actually gets the job done in your cells—is critically low. For a deeper dive into this issue, you can read more about the symptoms and challenges of low free testosterone.
This situation creates a hormonal illusion, where the lab report simply doesn’t match the reality of how you feel.
The Aromatization Problem
But that's not all. Hyperthyroidism creates another major problem by cranking up the activity of an enzyme called aromatase. This enzyme’s job is to convert your precious testosterone into estrogen. This process, known as aromatization, is a normal part of male physiology, but an overactive thyroid sends it into hyperdrive.
This creates a devastating one-two punch for your hormonal balance:
- Less Free Testosterone: Sky-high SHBG binds up and deactivates your available testosterone.
- More Estrogen: Overactive aromatase converts what little testosterone is left into estrogen.
This dramatic hormonal shift can trigger symptoms like gynecomastia (the development of male breast tissue), mood swings, and a further nosedive in libido. This isn’t just a theory; research confirms that in hyperthyroid men, SHBG surges and completely upends the testosterone-to-estrogen ratio.
Ultimately, looking at a single testosterone number without investigating the thyroid is a recipe for clinical failure. A truly accurate diagnosis demands a complete picture of how both systems are interacting. Only then can a clinician develop a treatment strategy that targets the real source of the problem and restores genuine hormonal health.
Decoding Your Labs: A Guide to Proper Testing
Trying to understand your health without the right data is like driving blind. To really grasp what’s happening between your thyroid and testosterone, you have to look beyond surface-level blood work and insist on a panel that tells the whole story.
Too often, standard check-ups only glance at one or two markers, like Thyroid-Stimulating Hormone (TSH) or Total Testosterone. While these are okay starting points, they give you an incomplete—and often misleading—picture of your hormonal health. Relying on them alone is why so many people get told "everything is normal" even when they know something feels off.
Beyond the Basics: Thyroid Testing
A single TSH test just shows the signal coming from your pituitary gland; it doesn't tell you how your thyroid is actually responding or if your body is using the hormones it’s making. To get a clear view, you need the full picture.
Here's what a complete thyroid panel should include:
- TSH (Thyroid-Stimulating Hormone): Measures the pituitary's "shout" to the thyroid. High levels can suggest your thyroid is struggling (hypothyroidism).
- Free T4 (FT4): Assesses the main inactive thyroid hormone that’s available to be converted into the active form.
- Free T3 (FT3): This is the money marker. It measures the active thyroid hormone that actually fuels your metabolism, energy, and mood.
- Reverse T3 (RT3): Checks for an inactive form of T3 that can clog up your receptors and block the active stuff from working. It's often elevated during periods of high stress.
- Thyroid Antibodies (TPO & TG): These detect an autoimmune attack on your thyroid, like Hashimoto's disease, which is the #1 cause of hypothyroidism in the U.S.
This comprehensive panel lets you see the entire production line—from the initial signal to the final, usable product. It helps pinpoint exactly where a breakdown is happening, which is absolutely critical for effective treatment. For a convenient alternative to traditional lab visits, our guide on how to check hormone levels at home offers some practical solutions.
The Complete Testosterone Picture
In the same way, a Total Testosterone test only tells you half the story. Like we’ve discussed, high levels of SHBG can lock up most of your testosterone, making it completely unusable. A thorough evaluation of the thyroid-testosterone connection demands a much more detailed hormone panel.
An accurate diagnosis hinges on seeing the full hormonal cascade. Without testing for free hormones, binding proteins, and estrogen, you're missing the key players that determine how you actually feel and function day-to-day.
To truly understand what's happening, we need to map out the entire system with a clear and comprehensive set of lab markers. This table breaks down the essential tests required for a full assessment of both thyroid and testosterone health.
Essential Lab Markers for Thyroid and Testosterone Health
| Lab Marker | What It Measures | Optimal Range (Example) | Why It's Important |
|---|---|---|---|
| TSH | Pituitary signal to the thyroid. | 0.5 – 2.0 mIU/L | Initial indicator of thyroid dysfunction (hypo- or hyperthyroidism). |
| Free T3 | The active, usable thyroid hormone. | Top 25% of lab range | Directly correlates with metabolic rate, energy, and mood. |
| Free T4 | The primary inactive thyroid hormone. | Mid-to-upper half of range | The reservoir of hormone available for conversion into active T3. |
| Thyroid Antibodies | Autoimmune attack on the thyroid. | Negative | Identifies autoimmune conditions like Hashimoto's, the leading cause of hypothyroidism. |
| Total Testosterone | All testosterone in the blood (bound + free). | Varies by age (e.g., 500-900 ng/dL) | Provides a baseline, but doesn't show what's actually usable by the body. |
| Free Testosterone | The unbound, bioavailable testosterone. | Top 25% of lab range | This is the hormone that drives libido, muscle mass, and energy. Arguably the most important T marker. |
| SHBG | The protein that binds to testosterone. | Lower half of lab range | High SHBG (common in hyperthyroidism) can drastically lower your Free T levels, causing symptoms. |
| Estradiol (E2) | The primary form of estrogen. | 20-30 pg/mL (for men) | The testosterone-to-estradiol ratio is crucial; imbalances can cause significant symptoms. |
| LH | Pituitary signal to the testes. | Varies by lab | Helps determine if low T is a primary (testicular) or secondary (pituitary) issue. |
With these comprehensive results in hand, you can finally move past the guesswork. You'll be equipped to have a productive, data-driven conversation with your doctor, ensuring your treatment plan is built on a complete understanding of your unique hormonal landscape.
Strategic Treatment: Fix The Thyroid First
When you’re staring down the barrel of both thyroid and testosterone problems, it’s easy to feel overwhelmed. But there’s a clear, logical order of operations here, and it’s built on a single, core principle: fix the thyroid first.
Trying to treat low testosterone while your thyroid is still out of whack is like trying to patch a leaky roof in the middle of a hurricane. You’re just chasing symptoms instead of getting to the root of the problem.
If hypothyroidism is the real domino that knocked over your testosterone, correcting it can be a total game-changer. Getting your thyroid levels right with proper medication allows your body’s entire hormonal signaling network to reboot. As your metabolism and cellular energy fire back up, the pituitary gland often gets back to its job of signaling the testes, and testosterone can climb back to healthy levels all on its own.
In a best-case scenario, this thyroid-first approach can eliminate the need for Testosterone Replacement Therapy (TRT) completely. For men whose testosterone issues are purely secondary to a struggling thyroid, getting that one piece right is often the complete solution.
Building a Stable Hormonal Foundation
Even if you have a separate issue like primary hypogonadism and genuinely need TRT, stabilizing your thyroid first isn't just a good idea—it's essential for the therapy to be safe and effective.
An unstable thyroid messes with how your body uses and responds to testosterone. This can make it incredibly difficult to dial in the right TRT dose, leaving you on a frustrating hormonal roller coaster with symptoms that never quite go away.
Think of it this way: your thyroid function is the foundation of your entire hormonal house. If that foundation is shaky, any other therapies you try to build on top of it are going to be compromised.
A smart treatment plan doesn't just chase numbers on a lab report; it works to restore the body's natural hormonal cascade. By prioritizing thyroid health, you create the perfect physiological environment for testosterone to recover on its own or for TRT to work exactly as it should.
Of course, medication isn't the only piece of the puzzle. Your lifestyle habits act as powerful co-factors, protecting your entire hormonal axis and amplifying the benefits of any medical treatment you’re on.
Essential Lifestyle Support for Hormone Health
To give your body the best shot at recovery, you need to integrate these supportive habits into your daily routine:
- Targeted Nutrition: Make sure your diet is loaded with the minerals essential for both thyroid and testosterone production. This includes selenium (Brazil nuts are a great source), zinc (found in lean meats and seeds), and iodine (from seaweed and dairy).
- Stress Management: Chronic stress floods your body with cortisol, a hormone that actively shuts down both thyroid function and testosterone production. Simple practices like meditation, deep breathing exercises, or even just a regular walk in nature can make a huge difference in keeping cortisol in check.
- Prioritize Sleep: Your body does most of its hormone production—including testosterone—during deep sleep. Getting a consistent 7-9 hours of quality sleep every night is non-negotiable for achieving hormonal balance.
By taking this strategic, whole-body approach, you connect all the dots. This method provides a clear and effective roadmap to achieving genuine, sustainable hormone optimization. For a deeper dive into recovery paths, check out our complete guide to low testosterone treatment options.
Got Questions? We Have Answers
When you're trying to figure out the connection between your thyroid and testosterone, it's easy to get lost in the details. Here are some straightforward answers to the questions we hear most often, designed to clear up the confusion and help you decide what to do next.
If I Fix My Thyroid, Will My Testosterone Come Back?
For a lot of guys, the answer is a definite yes. Since an underactive thyroid can put the brakes on the pituitary signals your body needs to make testosterone, getting your thyroid levels right with medication often reboots the whole system. This can lead to a major, sometimes even complete, recovery of your T levels without needing anything else.
Of course, this isn't a sure thing for everyone. The absolute first step is to get your thyroid function stable and optimized. That's the only way you and your doctor can see what your body's true testosterone baseline is once the thyroid is no longer holding it back.
Can I Take TRT and Thyroid Medication at the Same Time?
Absolutely. It’s actually quite common for someone to have two separate issues: hypothyroidism and primary hypogonadism (low T). When that's the case, treating both with thyroid medication and Testosterone Replacement Therapy (TRT) is the only way to truly feel your best.
This kind of dual therapy has to be managed carefully by a doctor who knows what they're doing. The dosage of one medication can affect how the other one works and how your body processes it. Regular, comprehensive blood work isn't just a suggestion—it's non-negotiable to keep both systems in balance and get you the relief you're looking for.
The goal of combined therapy is to create hormonal harmony. It requires meticulous monitoring to ensure that thyroid medication and TRT work together, not against each other, to restore your vitality and well-being.
Why Is My Total Testosterone High, but I Still Feel Awful?
This is a classic—and incredibly frustrating—sign of how an overactive thyroid messes with your hormones. When your thyroid is in overdrive, it can cause a huge spike in Sex Hormone-Binding Globulin (SHBG). SHBG is a protein that latches onto testosterone, basically locking it up so your body can't use it.
So, your lab report for "Total Testosterone" might look fantastic, maybe even impressively high. But the testosterone that actually matters—the usable "Free Testosterone"—is probably sitting in the basement. This is what causes those debilitating low T symptoms like crushing fatigue and a nonexistent libido. This scenario is the perfect example of why just testing Total T is not enough; you absolutely have to test for Free Testosterone and SHBG to get the real story.
Can I Improve My Thyroid and Testosterone with Diet and Exercise?
Yes, lifestyle is a huge piece of the puzzle for your entire endocrine system. While it's not likely to cure a diagnosed medical condition on its own, a solid lifestyle creates the perfect foundation for medical treatments to work their best and for your body to heal.
Think of it as building a strong support system:
- Nutrition: A diet rich in iodine, selenium, zinc, and vitamin D is non-negotiable for healthy thyroid function and testosterone production.
- Exercise: Hitting the weights is a game-changer. Resistance training is proven to give your testosterone a natural boost.
- Stress Management: Chronic stress floods your body with cortisol, which is toxic to both your thyroid and testosterone. Getting a handle on stress is crucial for protecting your hormonal balance.
By making these practices a regular part of your life, you're actively supporting the very foundation your hormonal health is built on. This makes any medical treatments you might need that much more effective.
At Elite Bioscience, we believe in giving you the tools to take control of your health. Our convenient at-home testing and physician-guided therapies are designed to provide clear answers and effective solutions for hormonal balance. Learn more about our personalized treatment options at https://elitebioscience.co.
QUICK SEARCH
Make an account today to start your journey towards a better and healthier lifestyle.