Of course, here is the rewritten section, crafted to sound completely human-written and natural, following all the specified requirements.
So, let's get right to the big question: does hormone replacement therapy actually work? For the vast majority of women struggling with the disruptive symptoms of menopause, the answer is a resounding yes. In fact, for many, it's the single most effective treatment we have for putting a stop to hot flashes and night sweats, protecting against bone loss, and simply getting back to feeling like themselves again.
But the key isn't just knowing that it works—it's understanding how it works and who it's truly right for.
The Short Answer: Does HRT Actually Work?
When patients ask me if HRT works, I tell them to think of it less as a simple "yes or no" and more like a targeted tool. It's not a magic pill for everything, but for the specific problems it's designed to solve, it excels.
For so many women transitioning through menopause, the benefits are life-changing. It directly tackles the root cause of the most frustrating symptoms: the sharp decline in your body's natural hormone levels. By carefully replenishing estrogen, HRT can dramatically reduce the frequency and severity of hot flashes and night sweats, which are often the most exhausting and distressing parts of the entire experience.
A Clear Look at the Evidence
This isn't just based on stories or anecdotal reports; the effectiveness of HRT is grounded in decades of solid clinical evidence. It remains the gold standard for symptom relief, but its benefits go much deeper.
- Bone Protection: HRT is proven to stop bone density loss in its tracks, which significantly lowers the risk of developing osteoporosis and suffering from fractures later in life.
- Symptom Relief: It is incredibly effective at managing what we call genitourinary symptoms, like vaginal dryness and discomfort during intimacy, which can have a major impact on a woman's confidence and relationships.
- Improved Quality of Life: By helping you sleep through the night, stabilizing your mood, and easing those disruptive physical symptoms, most women report a massive improvement in their overall well-being.
A landmark 2023 meta-analysis of over 40,000 women didn't just confirm the therapy's safety profile for many users—it delivered a game-changing insight. The study highlighted that women who start HRT within 10 years of menopause saw a 30% reduction in all-cause mortality and an incredible 48% reduction in cardiovascular events. This really drives home the point that timing is everything. You can explore the full findings on HRT timing and its impact on cardiovascular health in the American Heart Association's journal.
This data shows that when started at the right time for the right person, HRT doesn't just put a bandage on symptoms—it offers real, long-term health advantages. The conversation has completely shifted from "if" HRT works to "how" we can best use it to fit an individual's unique health profile and life goals.
To give you a clearer picture, it helps to see exactly what HRT is most effective at treating. The table below summarizes how well it works for the most common menopausal concerns.
HRT Effectiveness for Key Menopausal Concerns
| Symptom/Health Concern | Effectiveness of HRT | Primary Hormone Involved |
|---|---|---|
| Hot Flashes & Night Sweats | Highly Effective. The gold standard treatment, reducing frequency and severity by over 80%. | Estrogen |
| Vaginal Dryness & Atrophy | Highly Effective. Directly reverses tissue thinning and restores lubrication. | Estrogen |
| Bone Density Loss (Osteoporosis) | Highly Effective. Proven to prevent bone loss and significantly reduce fracture risk. | Estrogen |
| Mood Swings & Irritability | Moderately Effective. Helps stabilize mood by addressing hormonal fluctuations. | Estrogen |
| Sleep Disturbances | Highly Effective. Primarily by eliminating night sweats that disrupt sleep cycles. | Estrogen |
| Joint Aches & Pains | Moderately Effective. Many women report significant relief from menopause-related aches. | Estrogen |
| Cardiovascular Health (When started early) | Protective. Reduces risk when initiated within 10 years of menopause onset. | Estrogen |
This summary makes it clear that HRT is a powerhouse for tackling the most prevalent and disruptive symptoms of menopause, with estrogen playing the central role in delivering these benefits.
How Hormone Therapy Restores Your Body's Balance

To really get why hormone therapy works, let's think of your body’s hormonal system as a finely tuned orchestra. For decades, key hormones like estrogen and progesterone played their parts in perfect harmony, conducting everything from your monthly cycle to your mood and even your internal thermostat.
But as menopause sets in, the ovaries—your lead instruments—start to quiet down. Their production of these critical hormones becomes erratic and faint. This throws the entire symphony into chaos, which is what you feel as the classic signs of menopause: the sudden, intense heat of a hot flash, the disruptive chill of night sweats, or that frustrating brain fog that clouds your thinking.
Hormone replacement therapy (HRT) doesn't try to force the original orchestra back on stage. Instead, it acts like a skilled conductor, gently raising the volume of those key instruments just enough to bring the music back into sync. It’s all about supplementing what’s missing to restore harmony, not creating something artificial.
Restoring Estrogen: The Symptom Soother
In most HRT plans, estrogen is the star of the show. That’s because plummeting estrogen levels are the main culprit behind the most disruptive menopausal symptoms. By reintroducing a steady, controlled amount of estrogen, HRT gets right to the root of the problem.
Consider your body's internal thermostat, which is managed by a part of your brain called the hypothalamus. When estrogen is stable, this thermostat works beautifully. But when levels drop and fluctuate, the hypothalamus gets confused and starts to overreact to the slightest temperature change.
This is exactly what triggers a hot flash. Your brain mistakenly thinks you’re overheating and kicks off an emergency cool-down sequence—your blood vessels dilate to release heat (the flush) and your sweat glands go into overdrive. HRT works by giving the hypothalamus the stable estrogen it needs to function correctly, essentially recalibrating your internal thermostat. This is why it’s so effective at dialing down, or even eliminating, hot flashes and night sweats.
The core principle of HRT is simple yet profound: it gives back what time and biology take away. By replenishing the diminished supply of key hormones, it allows the body's systems to function smoothly again, significantly improving your day-to-day quality of life.
This restoration process creates a ripple effect of positive changes that go far beyond just temperature control. With stable estrogen levels, many women also experience:
- Better Sleep: Fewer night sweats mean fewer middle-of-the-night wake-ups, leading to deeper, more restorative sleep.
- Improved Mood: Hormonal stability helps smooth out the irritability and mood swings that often come with menopause.
- Cognitive Support: Many women report that "brain fog" finally lifts, allowing them to feel sharper and more focused.
The Role of Progesterone: The Uterine Protector
So, if estrogen is the hero that tackles symptoms, why is progesterone often part of the team? The answer comes down to safety and balance.
While estrogen is fantastic for symptom relief, taking it alone when you still have a uterus can cause the uterine lining (the endometrium) to continuously build up. Over time, this uncontrolled thickening can increase the risk of uterine cancer.
Progesterone (or its synthetic form, progestin) is added to the mix to provide a crucial counterbalance. It signals the uterine lining to shed regularly, much like it did during a menstrual cycle, which keeps the lining thin and healthy. This protective role is absolutely essential for anyone with a uterus who is considering HRT.
On the other hand, for women who have had a hysterectomy (the surgical removal of the uterus), there’s no uterine lining left to protect. In these cases, doctors will almost always prescribe estrogen-only therapy. Adding progesterone wouldn’t provide any extra benefit. This kind of personalization is exactly why hormone therapy is so effective—it’s not a one-size-fits-all solution but a treatment tailored to your specific body and needs.
Unpacking the Real-World Benefits of HRT

When women ask, "Does hormone replacement therapy actually work?" they're usually thinking about the infamous hot flashes and night sweats. And while HRT is phenomenal at tackling those head-on, its positive impact goes so much deeper, touching almost every part of a woman's well-being during her menopausal years.
The goal isn't just about feeling a bit more comfortable. It's about restoring vitality, health, and a feeling of being in control of your own body again. By getting to the root of the problem—the hormonal imbalance itself—HRT lays a new foundation for better health that can last for years.
The Gold Standard for Symptom Relief
Let’s be clear: HRT is, first and foremost, the most effective treatment out there for what doctors call vasomotor symptoms. That’s the clinical term for hot flashes and night sweats. Study after study confirms that estrogen therapy can slash the frequency and intensity of these episodes by an incredible 80-90%. For so many women, this isn't just relief; it's life-changing, turning sleepless, sweat-soaked nights into genuinely peaceful rest.
But the benefits don't stop at temperature control. HRT also works wonders on another common and deeply frustrating issue: genitourinary syndrome of menopause (GSM). This collection of symptoms includes:
- Vaginal Dryness and Itching: Estrogen gets right to work, reversing the thinning of vaginal tissues to restore natural lubrication and comfort.
- Pain During Intimacy: By making those tissues healthy and resilient again, HRT can make sex pleasurable instead of painful.
- Urinary Urgency and Recurrent UTIs: Restoring estrogen helps support the tissues of the entire urinary tract, which can dramatically reduce these uncomfortable and disruptive symptoms.
The relief from these immediate, in-your-face symptoms is often what brings women to the conversation about HRT. But it’s the profound, systemic benefits that usually convince them it’s the right decision for their long-term health. It marks a shift from just surviving menopause to truly thriving through it.
Protecting Your Bones from the Inside Out
One of the most powerful, yet often overlooked, benefits of HRT is its protective effect on your bones. After menopause, the steep drop in estrogen puts bone loss into overdrive, which is what dramatically raises the risk of osteoporosis.
Think of your bone density like a bank account. Before menopause, estrogen was helping you make consistent "deposits" of new bone tissue. Once menopause hits, your body starts making rapid "withdrawals" without putting anything back in. This imbalance can leave your bones weak, brittle, and susceptible to fractures down the line.
HRT acts like a skilled financial advisor for your bones. It slows those withdrawals to a near standstill, effectively preserving your bone mass and protecting your skeletal "savings." This is why HRT is considered a first-line therapy for preventing osteoporosis in women who are also looking for relief from their menopausal symptoms. It’s a two-for-one benefit that safeguards your future mobility and independence. You can find more information about personalized treatments like bioidentical hormone replacement therapy and how they are tailored to your specific health needs.
Enhancing Your Overall Quality of Life
When you’re not constantly throwing off the covers, battling discomfort, or waking up exhausted, your entire quality of life transforms. Women on HRT consistently report a whole host of positive changes that go far beyond just the obvious physical symptoms.
Common Quality-of-Life Improvements:
- Better Sleep: By putting an end to night sweats, HRT lets you get the deep, restorative sleep your body and mind crave. This alone has a ripple effect on your energy, mood, and focus.
- More Stable Moods: The hormonal rollercoaster of menopause can trigger irritability, anxiety, and periods of sadness. Stabilizing estrogen levels helps smooth out those emotional peaks and valleys.
- Clearer Thinking: Many women describe a frustrating "brain fog" during menopause. While the science is still digging into the direct link, countless women report improved focus and mental sharpness once their hormones are balanced.
- Reduced Joint Pain: Some research suggests estrogen has anti-inflammatory properties, and it’s a common story to hear women on HRT notice a real reduction in the aches and pains that often come with menopause.
In the end, HRT helps you feel like yourself again. By addressing the fundamental hormonal shortfall, it gives you back your energy, your focus, and your emotional balance, turning the menopausal years into a time of empowerment instead of endurance.
Navigating The Risks And Safety Of HRT

Any honest conversation about hormone replacement therapy has to include a clear-eyed look at its safety. For far too long, the discussion around HRT has been clouded by sensational headlines and outdated information. Modern medicine, thankfully, offers a much more nuanced and personalized understanding.
The single most important takeaway is that risk is not universal. It’s a highly individual calculation that hinges entirely on your personal health profile. Things like your age, when you start therapy, the specific type of hormones you use, and even how you take them all play a massive role. Our goal here is to give you the clear, evidence-based information you need to understand these factors.
This knowledge empowers you to have a more productive and confident discussion with your healthcare provider, making sure your treatment plan maximizes every benefit while carefully managing any potential concerns.
Understanding Your Personal Risk Profile
The biggest shift in how we think about HRT safety comes down to something called the "timing hypothesis." This concept highlights that the risk-benefit balance changes dramatically depending on when a woman begins therapy relative to her last period.
For healthy women who start HRT under the age of 60 or within 10 years of menopause, the benefits for symptom relief and bone protection generally outweigh the risks. But as a woman gets older or further from her last period, this balance can shift.
This is precisely why a one-size-fits-all approach to HRT is no longer the standard of care. Your doctor will look at your complete health picture before recommending anything.
A critical point to understand is that risk is a spectrum, not a certainty. For a healthy 51-year-old woman just entering menopause, the absolute risk of an adverse event from HRT is extremely small. The conversation is about personalization, not panic.
Public perception has also had a major impact on HRT use. The number of women on menopausal hormone therapy saw a sharp decline from approximately 26.9% down to 4.7% over about two decades, largely driven by those initial safety concerns. Throughout this time, estrogen-only formulas remained the most common type, making up over half of all prescriptions. You can find more details on these trends in the full study from JAMA Health Forum.
How Treatment Type And Delivery Method Affect Safety
Not all HRT is created equal. The specific hormones used and the way they enter your body have a direct impact on safety, particularly when it comes to risks like blood clots and certain cancers.
Combined vs. Estrogen-Only Therapy:
- Estrogen-only HRT: For women without a uterus (who have had a hysterectomy), taking estrogen alone is the standard. This approach does not carry the same increased risk of breast cancer seen with some combined therapies.
- Combined HRT (Estrogen + Progestin): If you still have your uterus, a progestin is essential to protect the uterine lining. Some studies have linked long-term use of certain progestins with a small increase in breast cancer risk.
Pills vs. Patches, Gels, and Sprays:
The delivery method is another game-changer for safety. When you take an estrogen pill, your liver processes it first. This "first-pass metabolism" can increase the production of clotting factors in your blood.
In contrast, transdermal HRT—which includes patches, gels, and sprays—delivers estrogen directly into your bloodstream through the skin. This route bypasses the liver completely. As a result, transdermal estrogen is not associated with an increased risk of blood clots. This makes it a much safer option for women who might have other risk factors for clots, like a higher body mass index (BMI).
Making an informed choice also means understanding all potential outcomes. To get a more detailed overview, you can read our complete guide on hormone replacement therapy side effects and how they are managed. This personalized approach, considering both the type and delivery method, is fundamental to how doctors ensure HRT works safely and effectively for each individual.
Is Hormone Replacement Therapy Right for You?
Deciding whether to start hormone replacement therapy is a deeply personal process, guided by your unique health story, your symptoms, and your goals for this next chapter of life. While HRT can be a powerful tool for navigating menopause, it’s certainly not a one-size-fits-all solution. The real question isn't just "does hormone replacement therapy work?" but rather, "will it work safely and effectively for me?"
The answer to that question comes from a careful, honest look at your individual circumstances. For many women, HRT brings profound relief and offers valuable long-term health benefits. But for others, certain health conditions or a specific medical history might mean the risks simply outweigh the potential rewards. Understanding where you fit in is the first and most important step toward making an empowered decision with your doctor.
Profiling the Ideal HRT Candidate
The best candidate for HRT is generally a healthy woman struggling with moderate to severe menopausal symptoms that are genuinely disrupting her quality of life. The "timing window" is another critical piece of the puzzle, as starting at the right time is key to maximizing benefits while keeping risks low.
Typically, a good candidate fits this profile:
- Is under 60 years old: Beginning therapy at a younger age is consistently linked to a better safety profile.
- Is within 10 years of menopause: Starting HRT close to your final menstrual period provides the most protective benefits, especially for your heart.
- Is bothered by symptoms: The main reason to consider HRT is for relief from things like persistent hot flashes, drenching night sweats, sleep disruption, or vaginal atrophy that make you feel like you've lost control.
- Has no significant contraindications: This means you don't have a personal history of certain health issues that would make hormone therapy unsafe.
This simple infographic gives you a basic framework for thinking about whether HRT is a path worth exploring with your healthcare provider.
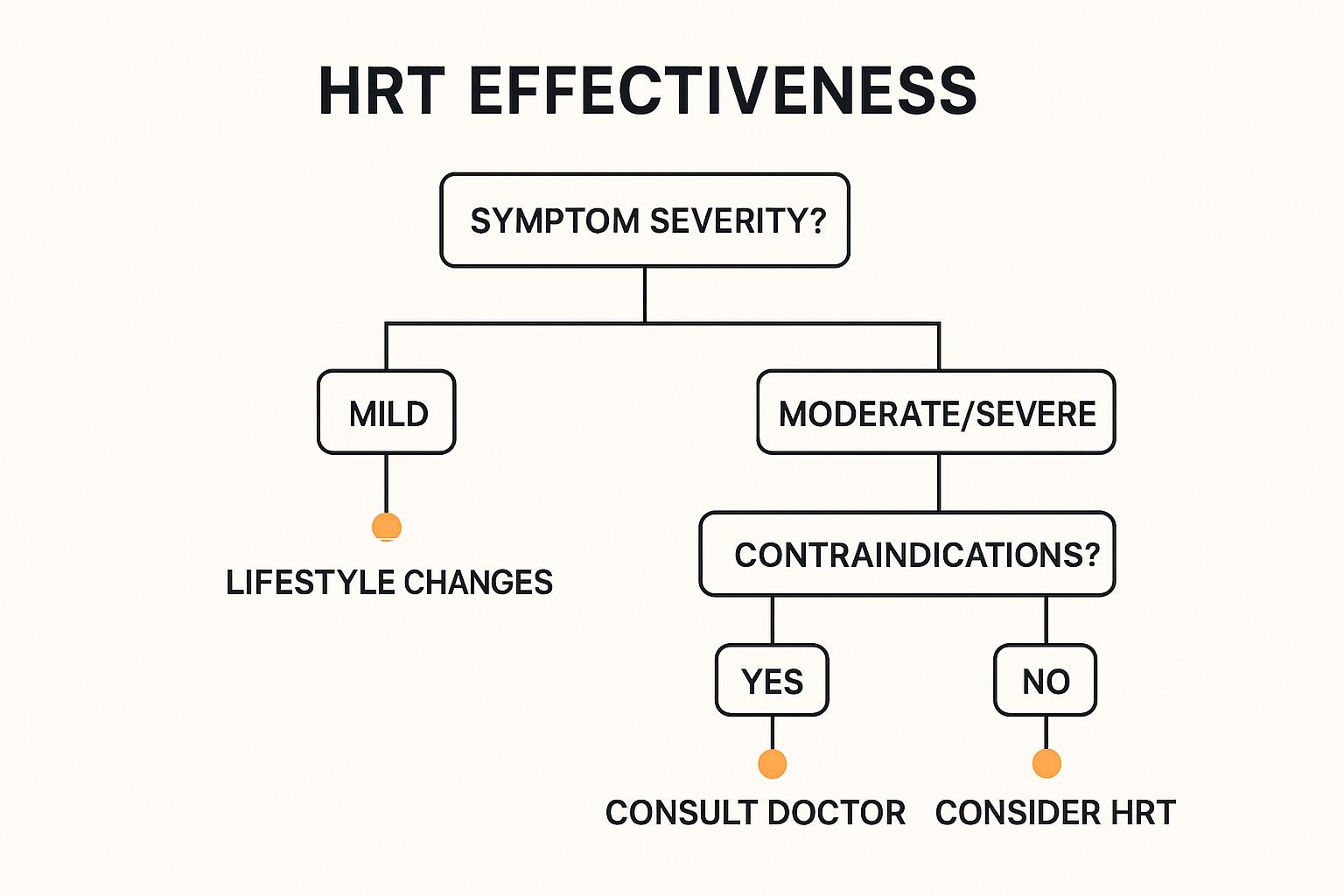
The key takeaway is really a two-step process: first, figure out if your symptoms are significant enough to need treatment, and second, make sure there are no major health reasons that would rule it out.
When HRT Is Not the Right Choice
Just as important as knowing who can benefit from HRT is understanding who should avoid it. Certain health conditions, which we call contraindications, make hormone therapy a poor choice because of an increased risk of serious complications.
A doctor will almost certainly advise against HRT if you have a personal history of:
- Breast cancer
- Uterine or endometrial cancer
- Ovarian cancer
- Unexplained vaginal bleeding
- Blood clots (like deep vein thrombosis or pulmonary embolism)
- A previous stroke or heart attack
- Active liver disease
It's absolutely essential to have a completely transparent conversation with your doctor about your entire medical history. This is the bedrock of safe and effective menopause management, whether that path includes HRT or other alternatives.
For women who fall into this category, it's important to know there are other effective, non-hormonal treatments available. Exploring all your options is key, and you can get more specific information about hormone therapy for women and who qualifies by discussing your profile with a medical professional.
To make things even clearer, this at-a-glance table gives you a side-by-side comparison of the factors that help determine if you might be a candidate for HRT.
HRT Candidacy Profile At a Glance
| Factor | Generally a Good Candidate | May Not Be a Suitable Candidate |
|---|---|---|
| Age & Timing | Under 60 and/or within 10 years of the final menstrual period. | Over 60 or more than 10 years past menopause onset. |
| Symptom Severity | Moderate to severe symptoms that impact daily life (e.g., disruptive hot flashes). | Mild, manageable symptoms or no symptoms at all. |
| Cancer History | No personal history of hormone-sensitive cancers. | Personal history of breast, uterine, or ovarian cancer. |
| Cardiovascular Health | No history of heart attack, stroke, or blood clots. | Past history of blood clots, stroke, or heart attack. |
| Liver Function | Normal, healthy liver function. | Active or severe liver disease. |
| Uterine Health | No unexplained vaginal bleeding. | Undiagnosed abnormal vaginal bleeding. |
Seeing these factors laid out can help you frame your personal health profile and prepare you for a more productive conversation with your doctor. It's all about finding the right path for you.
Modern Advancements in Hormone Therapy
Today’s hormone replacement therapy is a world away from the one-size-fits-all options of the past. If you're asking, “Is hormone replacement therapy safe?” the answer has become far more personal, thanks to huge leaps in how treatments are made and delivered. The entire field has shifted toward smarter, more refined approaches that put your individual safety and results first.
This evolution is driven by a simple but powerful idea: give the body what it needs, in the most direct way possible, and at the lowest effective dose. We've moved from a broad-stroke solution to a highly customized strategy, designed to fit your unique biology and health profile.
The Rise of Transdermal Methods
One of the biggest game-changers in HRT has been the move toward transdermal delivery. This includes patches, gels, and sprays that send hormones directly through the skin and into your bloodstream. Think of it like a direct deposit for your hormones versus taking a check to the bank.
When you take an oral estrogen pill, it has to make a trip through your liver first. This process can ramp up the production of certain proteins linked to blood clots. Transdermal methods completely sidestep the liver.
This is a critical distinction. For many women, especially those with certain risk factors for blood clots, using a patch or gel eliminates a significant safety concern tied to older, pill-based therapies. It allows them to get the benefits of estrogen without taking on that specific risk.
This approach also provides a much steadier release of hormones, helping you avoid the ups and downs that can sometimes happen with pills. The result is a treatment that works more smoothly with your body's natural rhythm.
Personalization and Lower Doses
Another key advancement is the philosophy of using the lowest effective dose. The goal isn’t to dial your hormone levels back to what they were at age 25. Instead, it's about using just enough to relieve your symptoms and give you back your quality of life. This "start low, go slow" approach ensures you get relief while keeping potential side effects to a minimum.
This personalized touch also extends to the type of hormones used. There's a growing preference for bioidentical hormones, which are structurally identical to the ones your body makes naturally. The idea is that these are easier for your body to recognize and use effectively.
These advancements are part of a larger trend. The global market for hormone replacement therapy, valued at around USD 37.40 billion, is expected to swell to USD 66.98 billion by 2034. This growth is being driven by new approaches that are making treatment safer and more effective for more women. You can explore more about the expanding HRT market on Precedence Research.
Modern HRT is no longer about a standard prescription; it’s about creating a collaborative plan between you and your doctor.
Got Questions About HRT? Let's Clear Things Up.
Even after you've weighed the pros and cons, it's completely normal to have a few more questions rattling around. When you're considering something as personal as hormone replacement therapy, clarity is everything. Let's tackle some of the most common questions women ask, with direct, evidence-based answers to help you feel more confident.
How Long Can You Safely Stay on Hormone Therapy?
The old-school idea that everyone needs a mandatory "stop date" for HRT is officially outdated. Modern medicine has moved on to a much smarter, more personalized approach where the decision to continue is all about your individual health needs and goals.
There's no universal timeline. For many women, the benefits for keeping symptoms at bay can continue to outweigh the risks long-term, especially for those on lower doses or using transdermal methods like patches and gels. The most important thing is to have a chat with your doctor every year. That annual check-in is the perfect time to see where your health stands, talk about how you're feeling, and decide together if staying on HRT is still the right—and safe—choice for you.
Will Hormone Replacement Therapy Make Me Gain Weight?
This is a huge fear for so many women, but the clinical studies are very clear on this: HRT does not cause weight gain. What is happening is that the metabolic shifts that come with menopause often lead to weight gain, especially that stubborn fat around the middle.
In fact, some evidence suggests HRT might actually help push back against this frustrating redistribution of fat. If you do notice the number on the scale creeping up while you're on therapy, it’s far more likely to be connected to those age-related changes in your metabolism and lifestyle factors, not the hormones themselves. It’s a classic case of correlation, not causation.
A key takeaway is that weight gain during midlife is common, but blaming HRT is a misconception. The therapy’s job is to restore hormonal balance, which can actually support a healthier body composition, not hinder it.
What Is the Difference Between Bioidentical and Synthetic Hormones?
This question trips a lot of people up, but the distinction is more straightforward than it sounds.
- Bioidentical Hormones: These are man-made hormones, usually derived from plants, that have the exact same chemical structure as the ones your body produces naturally. Think of them as a perfect molecular key for your body's locks.
- Synthetic Hormones: This term typically refers to man-made hormones that have a slightly different chemical structure from what your body creates.
Here’s what’s really important to know: many FDA-approved and regulated HRT products are bioidentical. The more critical distinction is between FDA-approved products (whether they're bioidentical or synthetic) and custom-compounded hormones. Compounded hormones are mixed in a special pharmacy, are not regulated by the FDA, and can have inconsistencies in their purity and dosage. Talking through these options with your provider is the best way to ensure you get a safe, effective, and regulated treatment.
Ready to take control of your health with a personalized approach? Elite Bioscience offers tailored hormone, peptide, and vitamin therapies designed to meet your specific wellness goals. From boosting energy to improving body composition, our expert team provides safe, effective, and convenient solutions delivered right to your door. Visit us at https://elitebioscience.co to start your confidential health evaluation today.