Hormone therapy for women is a medical treatment that replenishes the hormones your body isn't making enough of anymore, especially during menopause. It’s not about adding something foreign; it’s about restoring what’s missing to help you feel like yourself again and get relief from disruptive symptoms like hot flashes and night sweats.
What Is Hormone Therapy and How Does It Work
Think of your body’s hormones as a team of expert messengers, constantly sending signals to keep everything from your mood and energy levels to your sleep cycles running smoothly. During life stages like perimenopause and menopause, production of the key messengers—estrogen and progesterone—starts to drop off. This isn't just a minor change; it's a fundamental shift that can throw your body's entire system out of sync, leading to a cascade of unwelcome symptoms.
Hormone therapy for women works by stepping in to reintroduce these essential hormones and bring your body back into balance. It’s a targeted medical approach that replenishes what you’re missing, effectively recalibrating your internal communication network. By providing a steady, controlled supply of hormones, the therapy gets straight to the root cause of menopausal symptoms.
The Core Principle: Restoring Balance
The main goal here is simple: symptom relief and a better quality of life. When your estrogen levels are brought back to where they should be, it can dramatically reduce or even stop common issues like:
- Vasomotor Symptoms: This is the clinical term for those sudden, intense waves of heat from hot flashes and the drenching night sweats that can ruin a good night's sleep.
- Vaginal Health: Therapy can combat vaginal dryness, itching, and discomfort, which often impact intimacy and urinary health.
- Mood and Cognitive Function: Many women find that once their hormones are balanced, their mood stabilizes, irritability fades, and the frustrating "brain fog" starts to lift.
This process involves carefully prescribed hormones that are molecularly identical to the ones your body naturally creates. To learn more about how these plant-derived options closely mimic your own hormones, you can explore our guide on bioidentical hormone replacement therapy.
A Growing Field of Women's Health
More and more, hormone therapy is being recognized for the life-changing benefits it can provide, making it a major focus in women's health. The global market for these treatments is growing fast, reflecting a much greater understanding and acceptance of their role. The market was valued at around USD 19.7 billion and is expected to climb to USD 28.46 billion by 2029. You can explore more data on this growth trend in the full market report.
To simplify these concepts, here’s a quick overview of the therapy's main components.
Hormone Therapy for Women at a Glance
This table breaks down the core components of hormone therapy, including its goals, the key hormones involved, and the symptoms it is designed to address.
| Therapy Goal | Key Hormones Involved | Common Symptoms Addressed |
|---|---|---|
| Restore hormonal balance to alleviate menopausal symptoms. | Estrogen, Progesterone, and sometimes Testosterone. | Hot flashes, night sweats, vaginal dryness, mood swings, sleep disturbances. |
| Protect long-term health, particularly bone density. | Primarily Estrogen. | Prevention of bone loss and reduction of osteoporosis risk. |
| Improve overall quality of life and well-being. | A combination tailored to individual needs. | Low energy, "brain fog," reduced libido, and general discomfort. |
Ultimately, the aim is to use the right combination of hormones to restore balance, protect your long-term health, and help you feel your best.
Exploring the Types of Hormone Therapy
Deciding on hormone therapy isn't a one-size-fits-all choice. The world of hormone treatments is surprisingly diverse, with different formulations and delivery methods designed to fit your unique body and symptoms. Getting familiar with these options is the first step toward having a productive conversation with your provider about what’s right for you.
Think of it like watering a garden. Some plants need a deep, full-system watering that reaches every root, while others just need a gentle mist right on their leaves. Hormone therapy works in a similar way, offering both widespread and targeted solutions.
Systemic vs. Local Therapy
The most fundamental way we categorize hormone therapy is by how it works inside your body. The two main approaches are systemic and local therapy.
Systemic Hormone Therapy: This is the “full-system watering” approach. It circulates throughout your entire bloodstream to tackle widespread menopausal symptoms like hot flashes, night sweats, brain fog, and bone density loss. Systemic hormones come in various forms, including pills, patches, gels, and sprays.
Local Hormone Therapy: This is a more targeted approach, like misting a specific plant. It's applied directly to a particular area to treat localized issues—most commonly vaginal dryness, discomfort, or urinary symptoms. These treatments, like creams, tablets, or rings, use a much lower dose of hormones that primarily acts right where it’s applied, with very little absorption into the bloodstream.
The Two Core Formulations
Beyond how the hormones are delivered, the exact combination of hormones is crucial. Your personal health history—specifically, whether or not you have a uterus—will be the deciding factor in which formulation is right for you.
Hormone therapy remains the most effective treatment for vasomotor symptoms, which include the disruptive hot flashes and night sweats that many women experience during menopause.
Estrogen-Only Therapy (ET)
This approach involves taking only estrogen. ET is typically prescribed for women who have had a hysterectomy (the surgical removal of the uterus). Why? Because when taken on its own, estrogen can stimulate the growth of the uterine lining (the endometrium), which over time can increase the risk of uterine cancer.
Estrogen Plus Progestin Therapy (EPT)
For women who still have their uterus, this combination therapy is the standard of care. This treatment combines estrogen with a progestin (a synthetic form of progesterone) or progesterone itself. The progestin’s job is essential: it protects the uterus by keeping the uterine lining thin, effectively canceling out the risk associated with taking estrogen alone.
Bioidentical vs. Synthetic Hormones
Another key distinction you'll hear about is the difference between bioidentical and synthetic hormones. This can be a point of confusion, but the difference is actually pretty straightforward.
Bioidentical Hormones: These hormones are manufactured in a lab to be chemically identical to the ones your body produces naturally. Often derived from plant sources like yams or soy, they are structured to be a perfect key for your body’s hormone receptor locks.
Synthetic Hormones: These are also created in a lab, but their molecular structure is slightly different from the hormones your body makes. Premarin, one of the oldest forms of HRT, is a well-known example; it's derived from the urine of pregnant mares and is considered non-bioidentical.
While both types can be effective, many women and their doctors lean toward bioidentical options because they more closely mimic the body's natural processes. A clinician can help you weigh the pros and cons of each to find the perfect fit for your health profile and treatment goals.
The Real Benefits of Hormonal Balance

Finding hormonal balance is about so much more than just putting a stop to symptoms. It’s about truly reclaiming your vitality and protecting your health for the long haul. Hormone therapy for women delivers profound benefits, tackling both the immediate frustrations of menopause and the hidden risks that can surface later, helping you feel like yourself again.
One of the most life-changing benefits is powerful relief from those notorious vasomotor symptoms. The hot flashes that derail your day and the drenching night sweats that ruin your sleep can finally be managed. By replenishing estrogen, hormone therapy gets to the root cause of this internal thermostat malfunction, bringing you much-needed stability and comfort.
This renewed balance goes beyond just physical relief. It often leads to a massive improvement in mood and mental clarity. Many women describe it as the lifting of a persistent “brain fog,” allowing them to focus again, while also easing the irritability and mood swings that can feel so overwhelming.
Protecting Your Body for the Future
While the immediate symptom relief is fantastic, some of the most important benefits of hormone therapy are the ones working silently behind the scenes. Estrogen is critical for maintaining bone density. Its steep decline during menopause makes women highly susceptible to osteoporosis, a silent disease that weakens bones and makes them brittle.
By restoring estrogen levels, hormone therapy is a proven way to help prevent bone loss. This proactive measure can dramatically lower your risk of debilitating fractures down the road, safeguarding your mobility and independence for years to come.
This protective effect really highlights that therapy isn’t just a quick fix. It's a long-term investment in your future health, reinforcing your body’s foundational strength for the decades ahead.
Enhancing Quality of Life and Overall Wellness
When your hormones are in harmony, it touches nearly every part of your life. For instance, localized estrogen therapy can effectively address vaginal atrophy—reversing the dryness, itching, and discomfort that often make intimacy painful and can even affect urinary health. Restoring this delicate tissue improves both physical comfort and self-confidence.
Beyond that, hormone therapy can have a positive impact on other key areas:
- Energy Levels: So many women report a welcome return of their old energy and stamina.
- Skin Health: Estrogen is a key player in collagen production, which helps keep your skin hydrated and elastic.
- Libido: While sex drive is complex, restoring hormonal balance is often a crucial piece of the puzzle. While estrogen is a major factor, you can also explore the surprising benefits of testosterone therapy for women for a more complete picture.
Growth hormone is another piece of this complex puzzle. Though less common, growth hormone therapy has shown incredible results for women with certain conditions. For example, in girls with Turner syndrome and early estrogen deficiency, treatment led to an average adult height gain of about 9.59 cm more than what was expected without it.
Ultimately, achieving hormonal harmony is about getting your energy back, sharpening your mind, and feeling strong and vibrant again. It’s about being fully present and powerful in your own body.
Understanding the Risks and Side Effects

Let’s have an honest conversation about hormone therapy for women, and that means taking a clear-eyed look at the potential risks and side effects. For years, this topic has been clouded by confusion and fear, mostly stemming from early interpretations of major studies. Today, our medical understanding has evolved significantly, allowing for a much more personalized approach that weighs your unique benefits against any potential risks.
The most important thing to know is that risk isn't a simple, one-size-fits-all label. It’s a dynamic equation. Your personal risk profile is heavily influenced by your age when you start therapy, your overall health history, and the specific type, dose, and delivery method of the hormones you use.
Putting the Women's Health Initiative in Context
A lot of the lingering anxiety about hormone therapy traces back to the initial headlines from the Women's Health Initiative (WHI) study in the early 2000s, which linked therapy to increased health risks and sparked widespread fear. But with two decades of perspective, medical experts now see those findings in a much clearer light.
One of the most critical details is that the WHI study included a large number of older women, some already in their 70s, who were many years past the onset of menopause. We now understand that starting hormone therapy later in life carries a different risk profile than starting it during the menopausal transition. In fact, follow-up analyses have shown a very different picture for younger women (under 60 or within 10 years of menopause).
For most healthy women who begin hormone therapy early in their menopausal journey, the benefits—such as relief from debilitating symptoms and protection against bone loss—often outweigh the potential risks.
This modern understanding empowers you and your doctor to make a decision based on your specific life stage, not on outdated, generalized warnings.
Key Health Risks and Who Is Most Affected
While it’s a safe and effective option for many, hormone therapy does carry some serious risks that need to be carefully evaluated, particularly for certain individuals. The main concerns you and your doctor will discuss include:
- Blood Clots and Stroke: Systemic estrogen taken in pill form can slightly increase the risk of blood clots and stroke. This risk is lower with transdermal methods like patches or gels because they don't pass through the liver first.
- Heart Disease: Here, timing is everything. Starting therapy many years after menopause may increase heart-related risks, but starting closer to the transition does not appear to have the same effect.
- Breast and Uterine Cancer: For women who have a uterus, taking estrogen alone increases the risk of uterine cancer. That’s why combination therapy (estrogen plus progestin) is used to protect the uterine lining. The link to breast cancer is more complex and depends on the type of therapy and how long you use it.
This is exactly why a thorough medical history is non-negotiable. If you have a personal or strong family history of these conditions, hormone therapy might not be a safe choice for you.
To give you a clearer picture, this table shows how your individual health factors can influence your risk profile.
How Individual Factors Influence Hormone Therapy Risks
| Factor | Influence on Risk | Considerations for Your Doctor |
|---|---|---|
| Age | Starting under age 60 or within 10 years of menopause generally carries a lower risk profile. | Your doctor will assess whether the timing is appropriate and if the benefits outweigh risks for your age group. |
| Medical History | A personal or strong family history of breast cancer, heart disease, stroke, or blood clots significantly increases risk. | A comprehensive review of your personal and family medical history is essential to identify any red flags. |
| Type of Therapy | Estrogen-only therapy is for women without a uterus. Combination therapy (estrogen + progestin) is for women with a uterus. | The right formulation is chosen to protect you from specific risks, like uterine cancer. |
| Delivery Method | Pills (oral) carry a slightly higher risk of blood clots than patches, gels, or creams (transdermal). | Your doctor may recommend a transdermal method to minimize certain risks, especially if you have other risk factors. |
Understanding these nuances is the first step in creating a treatment plan that is both effective and right for your body.
Managing Common and Temporary Side Effects
Separate from the more serious risks, some women experience minor but manageable side effects, especially when first starting treatment. Think of it as your body adjusting to the new hormone levels—these often resolve on their own after a few weeks.
Common side effects can include:
- Bloating or fluid retention
- Breast tenderness or swelling
- Headaches or migraines
- Mood changes or irritability
- Nausea
These symptoms are often easily managed by adjusting the dose or changing the type of hormone or delivery method. It’s all part of the collaborative process with your provider to fine-tune your treatment until it feels just right.
How to Know If Hormone Therapy Is Right for You
Deciding whether to start hormone therapy for women is a deeply personal choice, one that hinges entirely on your unique health profile, symptoms, and where you are in life. The real question isn’t just about whether the therapy works in general—it's about whether it’s the right and safest choice for you. This decision is a true partnership between you and your healthcare provider, focused on carefully weighing the potential rewards against any personal risks.
The journey really starts with you. Take a moment for an honest self-assessment. Are your menopausal symptoms just a minor annoyance, or are they genuinely getting in the way? If things like hot flashes, night sweats, disruptive mood swings, or vaginal discomfort are actively wrecking your sleep, focus at work, or overall quality of life, then you might be a strong candidate. The primary job of hormone therapy is to relieve those moderate to severe symptoms that are holding you back.
The Ideal Candidate Profile
Medical guidance has identified a clear "window of opportunity" when hormone therapy is considered most beneficial and carries the lowest risk. Generally speaking, you’re likely a good candidate if you meet these criteria:
- You are under the age of 60. Starting therapy at a younger age is consistently linked to a better risk-to-benefit ratio.
- You are within 10 years of your last menstrual period. This is what experts call the "timing hypothesis," which suggests that beginning treatment closer to the onset of menopause offers the most protective benefits with the fewest risks.
- You are in good overall health. This means you don't have any major underlying conditions that would make hormone therapy an unsafe option.
For most healthy women who fit this description, the benefits of getting relief from their symptoms and protecting their bones long-term often clearly outweigh the potential risks.
The core principle here is that a personalized evaluation is everything. A treatment plan that’s perfect for one woman could be completely inappropriate for another, which is why a thorough discussion with a provider who sees your full health picture is non-negotiable.
Understanding Key Contraindications
Just as important as knowing who makes a good candidate is understanding who should avoid hormone therapy altogether. Certain medical conditions, known as contraindications, make this treatment unsafe. It's absolutely critical to be transparent with your doctor about your entire health history.
Hormone therapy is generally not recommended if you have a personal history of:
- Breast Cancer: A history of estrogen-sensitive cancers is a primary reason to avoid hormone therapy.
- Heart Disease or Stroke: If you've had a heart attack or stroke, the risks tied to hormone therapy may be too high.
- Blood Clots: A history of deep vein thrombosis (DVT) or a pulmonary embolism is a major contraindication.
- Unexplained Vaginal Bleeding: This must be investigated first to rule out serious underlying issues, like uterine cancer.
- Liver Disease: Since oral hormones are processed by the liver, significant liver dysfunction can be a major concern.
The Role of Personalized Medical Assessment
Ultimately, your own assessment is just the starting point. A true determination can only come from a professional medical evaluation. This will involve a deep dive into your symptoms, your personal and family medical history, and almost certainly some lab work to get a crystal-clear picture of your hormone levels. This data-driven approach is what ensures any treatment plan is built specifically for your body’s needs.
To see what this process actually involves, you can learn more about our comprehensive testing and analysis to determine appropriate dosages. This step is fundamental to creating a plan that is both safe and effective. Your provider will use all this information to help you make an informed decision, ensuring you feel confident and secure in whatever path you choose.
Starting Your Treatment Through Telehealth
In the past, starting hormone therapy for women meant scheduling clinic visits, taking time off work, and sitting in waiting rooms. Today, technology has made getting expert care more convenient and private than ever. With telehealth, you can manage your entire treatment journey right from home, connecting with experienced providers without ever stepping into a clinic. It’s a modern approach that makes world-class hormonal healthcare accessible, straightforward, and designed to fit your life.
The whole process is built for simplicity, kicking off with a confidential online consultation. You’ll fill out a health form that gives your provider a clear snapshot of your symptoms, medical history, and what you’re hoping to achieve. This first step is the foundation for creating a care plan that’s truly personalized to you.
Your Personalized Path to Treatment
After your initial online assessment, the next step is to get precise data on your unique hormonal landscape. This is where at-home testing shines, saving you a trip to a busy lab.
Comprehensive At-Home Testing: We mail a complete testing kit right to your door. Using just a simple blood spot sample, this kit accurately measures your current hormone levels. It gives your provider the critical information they need to understand exactly what your body needs.
One-on-One Virtual Consultation: Once we have your lab results, you’ll have a private, one-on-one virtual meeting with your dedicated healthcare provider. In this session, they will walk you through your results, explain what they mean in plain English, and answer every single question you have. Together, you’ll build a treatment plan that directly targets your symptoms and aligns with your health goals.
Discreet Doorstep Delivery: After the consultation, your prescribed medication is shipped discreetly to your home. No pharmacy visits, no waiting in line—your treatment arrives ready to use with clear instructions, respecting your privacy every step of the way.
This infographic lays out the simple, three-step journey to getting started with hormone therapy.
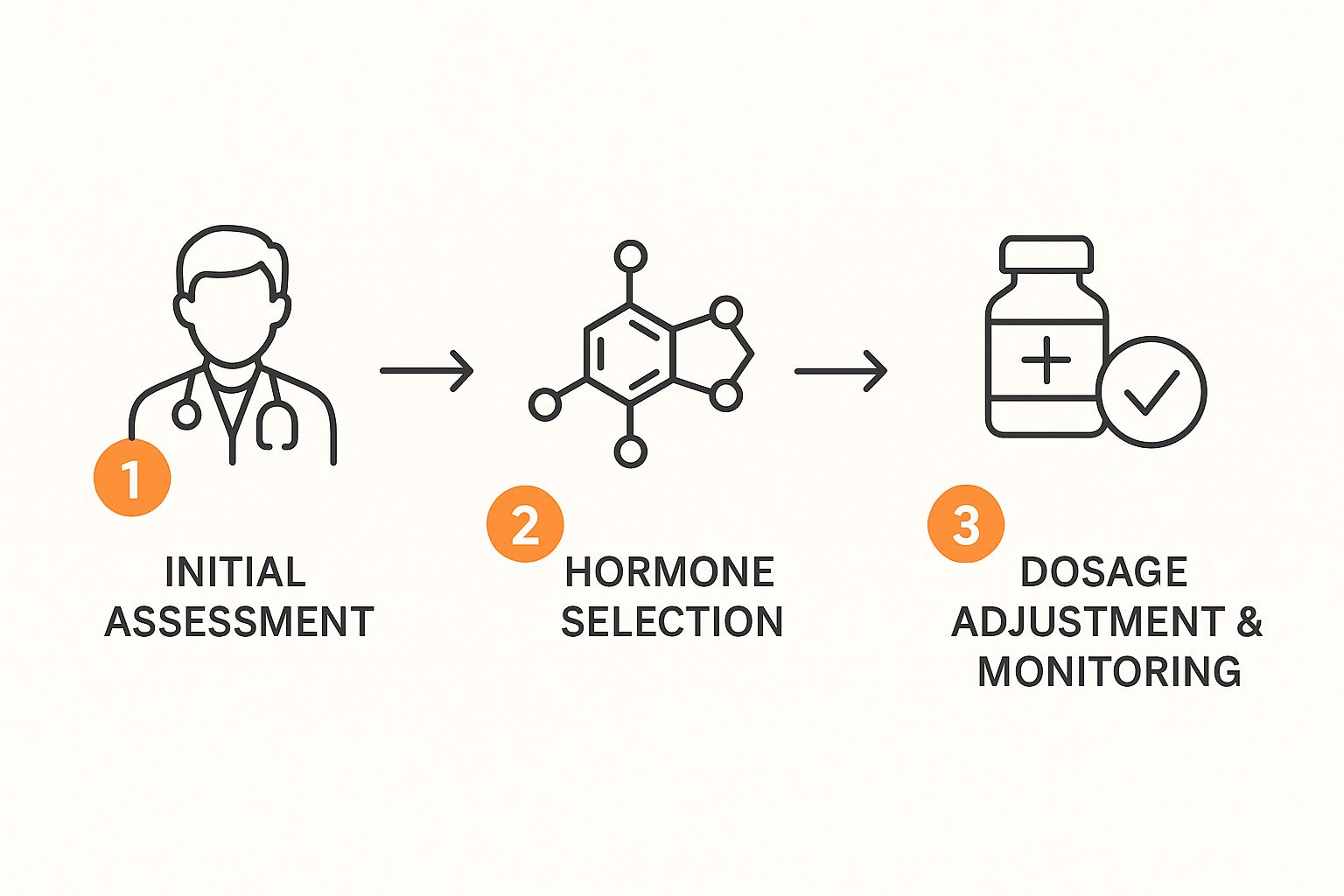
As you can see, the path to hormonal balance is a structured, logical progression from your initial assessment all the way to ongoing fine-tuning.
Ongoing Care and Fine-Tuning Your Plan
Your journey doesn't stop when your medication arrives. In fact, that’s really just the beginning of a supportive partnership with your provider. Consistent follow-up care is what ensures your treatment is not just working, but working optimally for your evolving needs.
The goal of ongoing care isn't just to maintain a treatment, but to perfect it. Small adjustments to your dosage or formulation can make a huge difference in how you feel, ensuring you get the best possible results while minimizing any potential side effects.
Regular check-ins are your opportunity to share feedback, and they allow your provider to monitor your progress and make any necessary tweaks. This continuous loop of feedback and refinement keeps your plan perfectly tuned to your body’s response. It’s this deep commitment to personalized, ongoing support that makes telehealth such a powerful and effective way to manage your hormonal health.
Common Questions About Hormone Therapy
Even after you've weighed the benefits and risks, it’s completely normal to have a few more questions rattling around in your head. Deciding on hormone therapy for women is a big step, and you deserve to feel confident and clear about the path forward. Let's tackle some of the most common questions we hear to help you understand the experience and set realistic expectations.
How Soon Will I Actually Feel Better?
This is usually the first thing women ask, and the honest answer is: it varies. Every woman's body is unique and will respond on its own timeline. However, many women report a noticeable drop in disruptive symptoms like hot flashes and night sweats within just a few weeks of starting treatment.
For other improvements—like a lift in your mood, more consistent energy, or better sleep—it might take a month or two for the full effects to kick in. Your body needs a little time to adjust to its new, stable hormonal environment.
How Long Can I Stay on Hormone Therapy?
This is a critical question, but there's no single, one-size-fits-all answer. The current medical thinking is to use the lowest effective dose for the shortest amount of time needed to manage your symptoms. For many women, this means using therapy to get through the most intense years of the menopausal transition.
However, the decision to continue or stop therapy is a personal one, made in an ongoing partnership with your provider. Your health will be re-evaluated regularly to make sure the benefits still outweigh any potential risks. Some women may choose to stay on a low dose of therapy for longer, especially for bone protection, and that's a perfectly valid conversation to have with your doctor.
What Happens If I Stop Taking It?
Deciding to come off hormone therapy should be a planned process, not a sudden stop. It's almost always recommended to taper off the medication slowly instead of quitting "cold turkey." This gradual reduction gives your body time to adjust and can help prevent a sudden, jarring return of symptoms like hot flashes.
While some women find their symptoms don't come back after stopping, others might notice them again, though often less intensely. If symptoms do return and start to disrupt your life, you can always revisit the conversation about restarting therapy or exploring other non-hormonal treatments with your provider.
Are Bioidentical Hormones Safer Than Traditional HRT?
The term "bioidentical" simply means the hormone is molecularly identical to the ones your body makes naturally. While this sounds great, it's important to know that "safer" isn't a straightforward concept here. All hormones, whether bioidentical or synthetic, carry risks and require a prescription and careful monitoring from a professional.
The biggest factor in safety often isn't whether a hormone is bioidentical, but how it's delivered. For instance, transdermal (through the skin) estrogen, which is bioidentical, is linked to a lower risk of blood clots compared to oral estrogen pills. The safest approach is always a personalized plan developed with an expert who looks at your complete health profile to choose the right hormone, dose, and delivery method just for you.
Ready to get personalized answers to your questions? The experts at Elite Bioscience are here to help you navigate your journey to hormonal balance with a tailored telehealth experience. Start your confidential online assessment today.