The Hidden Link Between Testosterone and Thyroid Health
The link between testosterone and thyroid hormones is one of the most important, yet often overlooked, relationships in your endocrine system. Think of them as two critical gears in a complex engine. If one slows down, or starts spinning out of control, it has a direct impact on the other—affecting everything from your energy and mood to your metabolism and muscle mass.
Getting this relationship right is absolutely essential for your overall well-being.
The Hormonal Orchestra: Testosterone and Your Thyroid
Picture your body’s hormonal network as a finely tuned orchestra. In this setup, the thyroid gland is the conductor, setting the tempo for your entire metabolism. It decides how fast your cells burn energy, which in turn controls your body temperature, heart rate, and overall vitality. When the conductor’s rhythm is off—either too slow (hypothyroidism) or too fast (hyperthyroidism)—the entire performance falls apart.
Now, think of testosterone as the powerful brass section of this orchestra. It’s the driving force behind key functions like:
- Building and maintaining muscle and bone
- Regulating sex drive and performance
- Supporting your mood, focus, and competitive edge
- Influencing the production of red blood cells
For the orchestra to sound incredible, the conductor and the brass section have to be perfectly in sync. If the thyroid’s tempo is sluggish, the testosterone section simply won’t have the energy or direction to play its part, leaving you with symptoms like crippling fatigue and a nonexistent drive.
On the other hand, if testosterone levels are low for other reasons, the body's overall power and strength diminish, which can drag down your metabolic health over time.
Before we dive deeper, let's establish a clear baseline. This table gives a quick snapshot of what each hormone system is primarily responsible for.
Quick Overview: Testosterone vs. Thyroid Hormones
| Hormone | Primary Gland | Key Functions |
|---|---|---|
| Testosterone | Testes (in men) | Muscle mass, bone density, libido, mood, red blood cell production |
| Thyroid Hormones (T3 & T4) | Thyroid Gland | Metabolism, energy regulation, heart rate, body temperature, growth |
As you can see, while their primary roles are distinct, they both have a huge impact on your body’s overall energy and function. Now, let’s explore exactly how they influence one another.
Why Their Interaction Is So Critical
This connection isn't just a clever metaphor; it’s grounded in your biochemistry.
One of the most crucial links involves a protein called Sex Hormone-Binding Globulin (SHBG). Your thyroid function directly tells your liver how much SHBG to produce. This matters because SHBG acts like a sponge, binding to testosterone in your bloodstream and making it unavailable for your body to use.
In other words, a dysfunctional thyroid can completely sabotage your free testosterone levels, even if your body is technically producing enough.
This isn't just a niche clinical finding. Large-scale studies have confirmed it across populations. For example, research analyzing large European cohorts found that even small increases in Thyroid-Stimulating Hormone (TSH)—a key marker of an underactive thyroid—were linked to a measurable drop in total testosterone. This shows that the intricate conversation between these two hormone systems is constant and critical. You can read the detailed findings of this genetic analysis to see the data for yourself.
Ultimately, you can't properly address one hormone without looking at the other. Understanding how they work together is the first step toward getting an accurate diagnosis and an effective treatment plan, ensuring every section of your hormonal orchestra is finally working in harmony.
The Science Behind Their Hormonal Crosstalk
To really get how testosterone and thyroid hormones are linked, you have to look at the intricate communication network that runs your body. Think of it like a complex shipping operation. Your hormones are the packages, and your bloodstream is the highway. But for a critical package like testosterone to be delivered and actually used, it needs a specialized transport vehicle.
This is where a protein called Sex Hormone-Binding Globulin (SHBG) comes in. Made mostly in the liver, SHBG acts like a fleet of armored cars for testosterone, binding to it and protecting it during its journey through the bloodstream. The catch? While testosterone is locked up with SHBG, it's inactive—it can't be used by your cells to build muscle, fuel your libido, or regulate your mood.
Only the testosterone that is not bound—what we call free testosterone—is biologically active and ready to get to work. And this is exactly where your thyroid’s influence becomes so critical.
Your Thyroid: The Dispatch Manager for Testosterone
Your thyroid function acts as the central dispatch manager for this entire hormonal shipping operation. It directly tells your liver how many SHBG "armored cars" to put on the road.
This relationship creates a delicate balance where even small shifts in thyroid function can send major ripples through your available testosterone levels.
-
Overactive Thyroid (Hyperthyroidism): When your thyroid is in overdrive, it sends a flood of signals to the liver, essentially shouting, "Deploy more trucks!" This leads to abnormally high levels of SHBG. With more trucks on the road, more testosterone gets locked away, causing a sharp drop in your free, usable testosterone. You might have plenty of total testosterone floating around, but your body simply can't access it.
-
Underactive Thyroid (Hypothyroidism): On the flip side, an underactive thyroid slows everything down. It tells the liver to scale back the SHBG fleet. Fewer trucks mean less bound testosterone, which might sound good, but it comes with the broader metabolic slowdown and other debilitating symptoms caused by the core thyroid problem.
This infographic helps visualize how these two essential hormone systems are meant to work together, supporting total body wellness, not as isolated systems.
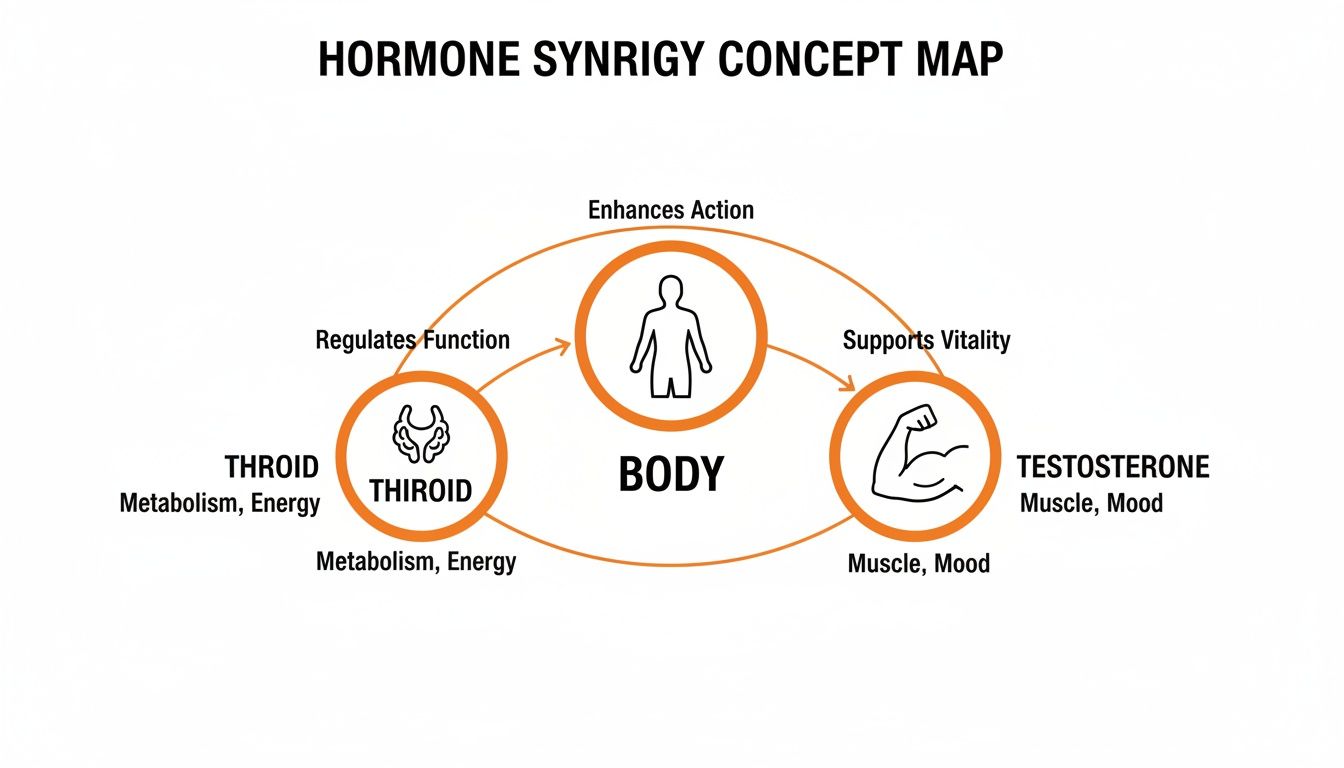
As you can see, both thyroid hormones and testosterone are foundational pillars of your overall health. When one starts to wobble, the other is sure to feel it.
The Brain’s Command and Control Centers
Beyond just SHBG, the connection between testosterone and thyroid goes all the way up to the brain, involving two parallel command-and-control pathways:
-
The Hypothalamic-Pituitary-Thyroid (HPT) Axis: This is the communication line for your thyroid. The hypothalamus releases a hormone (TRH) that tells the pituitary to release Thyroid-Stimulating Hormone (TSH). TSH then signals your thyroid gland, telling it how much hormone to produce.
-
The Hypothalamic-Pituitary-Gonadal (HPG) Axis: This is the pathway for testosterone. The hypothalamus releases a different hormone (GnRH) that signals the pituitary to release Luteinizing Hormone (LH). LH then travels to the testes and gives the command to produce testosterone.
These two axes are headquartered in the same regions of the brain—the hypothalamus and pituitary gland. Because they share a command center, a glitch in one system can easily disrupt the other.
For instance, severe or prolonged hypothyroidism can throw off the normal signaling within the pituitary gland. This can mess with the release of LH, directly weakening the signal for testosterone production. This can lead to what's known as secondary hypogonadism—a condition where the testes are perfectly healthy but just aren't getting the command to make enough testosterone.
This intricate biological crosstalk is precisely why it's impossible to properly evaluate one hormone without looking at the other. A problem that shows up as low testosterone might actually have its roots in a sluggish thyroid, and vice versa. Understanding this fundamental science is the first step toward getting an accurate diagnosis and finally restoring true hormonal balance.
Decoding Overlapping and Confusing Symptoms
Are you feeling completely drained, gaining weight no matter what you do, and noticing your libido has taken a nosedive? Trying to pinpoint the cause can feel like you're lost in a maze. The symptoms of low testosterone and an underactive thyroid often blur together, creating a confusing clinical picture that’s tough to solve without professional help.
This symptom overlap is precisely why understanding the testosterone and thyroid connection is so critical. It's a common pitfall to blame all your symptoms on one issue while the other goes completely unchecked, which only delays effective treatment and leaves you feeling stuck and frustrated.

Think of it like a warning light on your car's dashboard. Two different engine codes are triggering the exact same light. You might fix the first problem you find, but the light stays on because the second issue is still there. This is exactly what happens with hormonal imbalances.
The Venn Diagram of Feeling Awful
To get some clarity, let’s break down the symptoms into three distinct buckets: those that point strongly to low testosterone, those that are classic signs of hypothyroidism, and the big group of symptoms that sit right in the middle.
Symptoms That Scream "Low Testosterone"
- Losing muscle mass and strength, even though you’re still hitting the gym.
- A nosedive in your libido or a major drop in sexual desire and performance.
- Trouble getting or maintaining erections—a classic hallmark of low T.
- Less body and facial hair growth, which is a direct reflection of declining androgen activity.
Symptoms That Point to a Sluggish Thyroid
- Feeling cold all the time, especially when everyone else feels comfortable.
- Dry, coarse skin and brittle nails, which happens when a slow metabolism affects skin cell renewal.
- Constipation, because a sluggish metabolism slows down your digestive system, too.
- A puffy face or hoarseness in your voice, often caused by fluid retention common in thyroid disorders.
This separation helps, but the real diagnostic headache comes from the symptoms these two conditions share.
Symptom Checker: Low T vs Low Thyroid
It can be tough to tell these conditions apart based on feelings alone. This table breaks down which symptoms are most commonly linked to each condition, helping you see where the biggest overlaps occur.
| Symptom | Common in Low Testosterone | Common in Hypothyroidism |
|---|---|---|
| Fatigue & Low Energy | Yes (Often mental/physical) | Yes (Often deep exhaustion) |
| Weight Gain | Yes (Especially belly fat) | Yes (Often all over) |
| Depression & Mood Swings | Yes (Irritability, apathy) | Yes (Sadness, lethargy) |
| Brain Fog/Poor Focus | Yes | Yes |
| Low Libido | Yes (Primary symptom) | Yes (Often secondary to fatigue) |
| Muscle Aches & Weakness | Yes | Yes |
| Erectile Dysfunction | Yes (Hallmark symptom) | Sometimes |
| Cold Sensitivity | No | Yes (Hallmark symptom) |
| Dry Skin & Brittle Nails | No | Yes (Hallmark symptom) |
| Constipation | No | Yes (Hallmark symptom) |
While this table offers a guide, it’s not a substitute for a real diagnosis. The significant overlap, especially with major quality-of-life symptoms like fatigue and depression, shows why comprehensive lab work is absolutely necessary.
The Overlap Zone: Where Symptoms Collide
Many of the most frustrating symptoms can be caused by either low T, hypothyroidism, or—very often—both at the same time. This is where trying to self-diagnose becomes a guessing game and where comprehensive lab testing is non-negotiable.
The most common shared symptoms—fatigue, weight gain, and depression—are often the ones that most impact a person's quality of life. Mistaking one condition for the other can lead to ineffective treatment and continued suffering.
Here’s a closer look at the most common signs that live in this confusing middle ground:
- Persistent Fatigue and Low Energy: This isn’t just being tired after a long day. It’s a chronic, bone-deep exhaustion that a good night’s sleep just can’t fix.
- Unexplained Weight Gain: Both hormones are metabolic powerhouses. When their levels are low, your body’s calorie-burning engine slows to a crawl, making it incredibly easy to gain weight, especially around your midsection.
- Depression and Mood Swings: Hormones are powerful mood regulators. When they’re out of balance, it can lead to feelings of sadness, irritability, and a total loss of interest in things you used to enjoy.
- Brain Fog and Poor Concentration: Both conditions can mess with your cognitive function, making it hard to focus, remember details, or think with any clarity.
Because this list of shared symptoms is so long, a detailed medical workup is the only way forward. For instance, while low libido is a primary symptom of low T, it can also be a side effect of the crushing fatigue and depression caused by hypothyroidism. A key piece of the puzzle is understanding how free testosterone—the active, usable form in your body—is affected. To learn more, check out our guide to understanding low free testosterone.
How Thyroid Dysfunction Sinks Testosterone Levels
Now that we've seen how the symptoms can look eerily similar, let's get into the mechanics. A struggling thyroid doesn't just mimic low T—it can be the direct cause of your testosterone crash. Whether your thyroid is running too slow or too fast, it kicks off a chain reaction that throws your entire hormonal system out of whack.
This isn't just a random correlation; it's a predictable biological outcome. Think of your thyroid as the engine setting your body's metabolic pace. When that pace is off, it directly messes with how testosterone is produced, transported, and actually used by your cells.
The Underactive Thyroid Domino Effect
When your thyroid is underactive (hypothyroidism), your whole system grinds to a slower, sluggish pace. This metabolic slowdown can trigger what’s known as secondary hypogonadism. In simple terms, this means your testes are perfectly fine and ready to work, but they aren't getting the right orders from headquarters—your brain.
Here’s how that domino chain falls:
- Pituitary Glitch: A long-term sluggish thyroid can interfere with the pituitary gland, the brain's hormonal command center.
- Signal Fades: This disruption weakens the release of Luteinizing Hormone (LH), which is the specific signal that tells your testes to get to work producing testosterone.
- Production Halts: With a weak, flickering signal coming from the brain, your testes dial down production, leading to low T and all the symptoms that come with it.
Basically, your testosterone factory is fully operational, but the manager (the pituitary) is too bogged down to send out the production memos. This is a textbook case of how a problem in one hormonal system can cause a total breakdown in another.
This uncovers a crucial rule in hormone diagnostics: If a man shows up with low T symptoms and his labs confirm secondary hypogonadism, running a full thyroid panel is non-negotiable. Often, fixing the underlying thyroid problem is all it takes to get testosterone production back online naturally.
The Overactive Thyroid Paradox
An overactive thyroid (hyperthyroidism) causes a different, but just as frustrating, problem. It creates a confusing situation where your total testosterone might look normal—or even high—on a lab report, yet you feel every single symptom of low T. This happens because of a massive spike in Sex Hormone-Binding Globulin (SHBG).
As we've covered, SHBG is a protein that latches onto testosterone and renders it useless. An overactive thyroid sends SHBG production into hyperdrive.
This leaves most of your testosterone shackled and unavailable for your body to use. Your free testosterone—the stuff that actually fuels your muscle, mood, and sex drive—plummets. It’s like having a million dollars in the bank but no ATM card to access any of it.
The impact of thyroid disease on these hormones is clear and measurable. In cases of untreated hyperthyroidism, studies show significant jumps in SHBG, sometimes by 50% or more. This artificially inflates total testosterone while free testosterone may stay in the normal range. Hypothyroidism does the opposite, often lowering SHBG and making low total testosterone numbers look even worse. You can explore the research on thyroid disease and sex hormones to see the data for yourself.
A Real-World Example
Take Mark, a 42-year-old who felt completely wiped out. His focus was shot, he’d gained 15 pounds even though he was hitting the gym, and his sex drive was gone. His first labs showed his total testosterone was borderline low, but his doctor knew to look deeper.
A full thyroid panel revealed the real culprit: Hashimoto's disease, a common autoimmune disorder that causes hypothyroidism. His TSH was sky-high, confirming his thyroid was failing. Instead of jumping to TRT, his doctor focused on treating the thyroid first.
Three months after starting thyroid medication, Mark's energy was back, the brain fog had cleared, and his mood was stable. A new blood test showed his LH signals were firing properly again, and his testosterone levels had climbed back into a healthy range—all without a single testosterone shot. Mark's story is a perfect example of why the root of low T is so often found in the thyroid.
How Testosterone Therapy Can Affect Your Thyroid
While a struggling thyroid can tank your testosterone, this relationship is a two-way street. Starting Testosterone Replacement Therapy (TRT) can, in turn, influence how your thyroid functions and how your body uses its hormones. This is a critical piece of the puzzle for anyone managing both conditions, as TRT can shift your hormonal balance in ways you might not expect.
The key to this interaction is another transport protein called Thyroxine-Binding Globulin (TBG). Think of TBG as the dedicated delivery service for your thyroid hormones, T4 and T3. It’s responsible for carrying them through the bloodstream to every single cell in your body.
Just as your thyroid can influence SHBG (the testosterone taxi), your testosterone levels can influence TBG. When you introduce external testosterone through TRT, it can change the amount of TBG in your system, which directly impacts how your thyroid hormones are delivered and used.
The Impact on Thyroid Medication
This interaction is especially important for men already taking thyroid medication, like levothyroxine, for hypothyroidism. For them, starting TRT can significantly alter how the body responds to their prescribed thyroid hormone dose.
TRT has been shown to decrease the concentration of TBG in the bloodstream. With fewer TBG "delivery trucks" available, more thyroid hormone is left unbound and "free" to be used by your cells. Suddenly, your current thyroid medication dose could become far too strong.
This isn't just a minor tweak; it can be enough to trigger symptoms of an overactive thyroid (hyperthyroidism), such as:
- Anxiety, restlessness, or irritability
- Heart palpitations or a racing pulse
- Increased sweating and heat intolerance
- Unexplained weight loss
All of a sudden, the medication that was perfectly balanced to manage your hypothyroidism might push you into the opposite extreme, all because of the introduction of TRT.
Key Takeaway: Therapeutic interventions for one hormonal system frequently affect the other. Since TRT can decrease TBG, men with hypothyroidism may need a reduction in their levothyroxine dose after starting therapy to avoid becoming overmedicated. As clinical guidance suggests, this adjustment is often necessary to maintain stable thyroid hormone levels.
The Need for Careful Monitoring
This dynamic is exactly why a siloed approach to hormone therapy is so risky. Treating low testosterone without considering its effect on the thyroid—or vice versa—can lead to a frustrating cycle of chasing symptoms and constantly adjusting medications.
It is absolutely essential that your thyroid levels are re-evaluated after you begin TRT, especially if you're on thyroid medication. This isn't a "one-and-done" test. Your clinician should be monitoring your full thyroid panel (TSH, Free T4, and Free T3) approximately 6-8 weeks after starting therapy and after any significant dose adjustments.
This proactive monitoring allows your healthcare provider to make informed decisions, ensuring both therapies work together harmoniously. By carefully managing both the testosterone and thyroid connection, you can achieve true hormonal balance and finally feel your best. This is a core principle behind effective treatments, including options like testosterone replacement therapy at home, which must always be managed under expert medical supervision.
The goal isn't just to treat two separate issues; it's to create a cohesive treatment plan where both hormonal systems are supported. This prevents one therapy from unintentionally sabotaging the other and ensures your path to wellness is as smooth and successful as possible.
Securing an Accurate Diagnosis with the Right Lab Tests
When you're dealing with a confusing mess of overlapping symptoms, the last thing you want is guesswork. A real diagnosis for issues involving testosterone and thyroid hormones has to be built on a solid foundation of comprehensive lab data. It's a common trap: treating one condition while another, related problem goes unnoticed, leaving you stuck with persistent symptoms and a whole lot of frustration.
Because things like fatigue, weight gain, and a nosedive in your libido can point to either system, testing both at the same time is non-negotiable. This strategy gives your doctor a complete hormonal snapshot, allowing them to see the full picture and pinpoint the actual root cause of what's going on, instead of just chasing symptoms one by one.
Key Lab Markers for Testosterone
To really understand your testosterone status, you have to look beyond just one number. A complete picture requires evaluating a few interconnected markers that tell a much more detailed story.
- Total Testosterone: This measures every bit of testosterone in your bloodstream, both the stuff that's bound up and the stuff that's free. It’s a decent starting point, but it definitely doesn't tell the whole story.
- Free Testosterone: Now we're talking. This is the biologically active, usable testosterone that isn’t attached to proteins. It’s a far better indicator of how you actually feel.
- Sex Hormone-Binding Globulin (SHBG): Think of this as a protein that grabs onto testosterone and puts it on the sidelines, making it inactive. High SHBG can give you all the symptoms of low T even if your total testosterone looks perfectly normal. You can easily order a comprehensive testosterone test online to check these levels from home.
Essential Thyroid Function Tests
In the same way, a proper thyroid evaluation needs more than just a single test. The following markers give you critical insight into how the entire thyroid system is firing.
- Thyroid-Stimulating Hormone (TSH): Think of TSH as the message your brain sends to your thyroid. A high TSH is like your brain shouting at a sluggish thyroid to get to work, which is a classic sign of potential hypothyroidism.
- Free T4 (Thyroxine): This is the main storage hormone the thyroid gland produces. Measuring the "free" level shows how much is actually available for your body to convert into the active form.
- Free T3 (Triiodothyronine): This is the active thyroid hormone that directly revs up your metabolism and dictates your energy levels. Low levels here can explain why you feel so run-down.
When you look at both sets of labs together, a clear pattern often starts to emerge. For example, seeing low free testosterone paired with high SHBG and a high TSH strongly suggests that an underactive thyroid is the primary driver of the problem. This is the kind of insight that empowers you to advocate for the right kind of testing and ensures you get a treatment plan that actually works.
Your Questions Answered
When you're trying to figure out the connection between testosterone and thyroid health, a lot of practical questions come up. Let's tackle the most common ones head-on, giving you the clear answers you need to have a smarter conversation with your doctor.
Can Treating My Hypothyroidism Naturally Increase My Testosterone?
In many cases, yes, it absolutely can. If a sluggish thyroid is the real culprit behind your low T (a classic case of secondary hypogonadism), then fixing the root cause is often the only fix you need.
When you get your thyroid levels dialed in with the right medication, it allows your pituitary gland to send the right signals again and helps normalize your SHBG levels. This process can kickstart your body's own testosterone production, sometimes bringing it all the way back to a healthy range without ever needing a drop of TRT. It's exactly why any good clinician will treat a diagnosed thyroid problem first, then circle back to check your testosterone once things have leveled out.
The smartest play is always to fix the foundation first. When you restore proper thyroid function, the body's entire hormonal system gets a chance to reset, which often makes direct testosterone therapy unnecessary.
What Should I Expect If I Start Thyroid Medication While on TRT?
If you're already on a stable TRT protocol and then start taking thyroid medication like levothyroxine, get ready for some adjustments. This is a big deal, and you'll need to work closely with your doctor.
Starting thyroid hormone will almost certainly change how your body uses testosterone. It can raise your SHBG, which acts like a sponge, binding up more of your testosterone and leaving less "free" T available for your body to actually use. You could suddenly find your old low T symptoms creeping back, even though your TRT dose hasn't changed.
Your doctor will need to run a full thyroid panel and a complete testosterone panel (Total T, Free T, and SHBG) about 6-8 weeks after you start the new medication. This isn't optional—it's the only way to see what's really going on and figure out if your TRT dose needs to be tweaked to get you back in balance.
Which Doctor Should I See: A Urologist or an Endocrinologist?
While a urologist is often the go-to for managing TRT, an endocrinologist is a specialist in the entire hormonal orchestra—the endocrine system. This includes everything from the thyroid gland in your neck to the testes that produce your testosterone.
When you’re dealing with a complex puzzle involving the direct interplay between testosterone and thyroid function, an endocrinologist is usually the most qualified expert. They have the deep training needed to see the whole picture, run the right diagnostics, and build a cohesive treatment plan that balances both systems perfectly, ensuring one therapy doesn't accidentally sabotage the other.
Take control of your hormonal health with a modern approach. At Elite Bioscience, we provide medically supervised hormone therapies delivered directly to you, making it simple to get the expert care you need. Explore our tailored treatment options today.
QUICK SEARCH
Make an account today to start your journey towards a better and healthier lifestyle.