Is TRT Covered by Insurance? A Practical Guide

So, does insurance actually cover TRT? The short answer is yes, often it does—but with a big catch. It has to be proven medically necessary.
Coverage isn't for a lifestyle boost or for the normal side effects of aging. It's for treating a diagnosed medical condition known as hypogonadism.
Understanding The Basics Of TRT Insurance Coverage
Think of getting TRT covered like getting prescription glasses. Your insurer will gladly pay for lenses after an optometrist provides hard proof of poor vision. But they won't cover a stylish pair of non-prescription frames just because you want them.
It's the same deal with testosterone therapy. Your insurance company needs concrete, objective evidence before they'll sign off on it. This means you and your doctor have to build a solid case based on specific, measurable criteria. Vague complaints about feeling tired or less energetic just won't cut it. They’re looking for a clear combination of documented symptoms and, most importantly, conclusive lab work.
Core Requirements For Approval
Almost every insurance plan boils its decision down to two main factors:
- Clinically Low Testosterone Levels: Insurers demand multiple blood tests to prove your testosterone is consistently below their threshold. These are usually taken first thing in the morning when your levels are at their peak. For most, this means a reading under 300 ng/dL.
- Documented Medical Symptoms: Your doctor needs to have a record of specific symptoms directly linked to hypogonadism, like severe fatigue, loss of muscle mass, or a noticeable drop in libido.
The U.S. TRT market pulled in USD 736.1 million in 2024 and is still climbing. A big reason for this growth is that insurers are increasingly recognizing clinically diagnosed hypogonadism as a legitimate medical condition that requires treatment. You can find more insights on the TRT market and its insurance trends.
Figuring all this out can feel a bit overwhelming, and it's smart to understand the financial side of things, especially when you look at the cost of TRT without insurance.
To make it easier, here’s a quick checklist summarizing what most insurance companies are looking for.
Quick Checklist for TRT Insurance Coverage
This table breaks down the three core pillars that insurers use to determine medical necessity for TRT. Getting these three things lined up is your best shot at getting your treatment approved.
| Requirement | What It Means | Why Insurers Care |
|---|---|---|
| Lab-Confirmed Low T | Multiple blood tests showing testosterone consistently below the 300 ng/dL threshold. | This provides objective, scientific proof of a deficiency, removing any subjective guesswork. |
| Physician Diagnosis | An official diagnosis of hypogonadism from a qualified doctor. | It confirms the condition is a recognized medical issue, not just a lifestyle choice. |
| Documented Symptoms | Your medical records must detail specific symptoms clearly linked to low testosterone. | This connects the lab results to real-world health impacts, justifying the need for treatment. |
Having these three elements in your medical file creates a strong, clear case for why TRT is a medical necessity for you, not just a preference.
Proving Medical Necessity for Your TRT Claim
To get your TRT covered by insurance, you and your doctor need to build an ironclad case for medical necessity. This isn't about just feeling a little off your game; it's about connecting two critical pieces of the puzzle: conclusive lab results and a clear clinical picture of your symptoms.
Think of your insurance provider as a judge and your claim as the case file. Without rock-solid evidence, the verdict is almost always going to be "denied." Insurers need objective proof, not just how you feel on a given day.
The Two Pillars of Proof
The first piece of evidence is your blood work. Insurance companies almost universally require a series of early-morning blood tests showing testosterone levels that are consistently below their specific threshold. This cutoff usually hovers around 300 ng/dL. A single low reading often isn't enough; they want to see a persistent deficiency. Understanding these numbers is vital, and you can learn more about how to read lab results to better prepare for those conversations with your doctor.
The second pillar is the documented presence of specific, significant symptoms. We're not talking about vague complaints here. Insurers are looking for medically recognized signs of clinical hypogonadism, which include things like:
- Severe and persistent fatigue that gets in the way of your daily life
- Documented loss of muscle mass and strength
- Clinically diagnosed depression or other mood disorders
- A significant and sustained drop in libido
This is where the real distinction lies. Insurance covers treatment for a diagnosed medical condition—clinical hypogonadism. They do not cover treatment for the natural, gradual decline in testosterone that simply comes with getting older.
This decision tree gives you a simple look at the core logic insurers use when they evaluate a TRT claim.
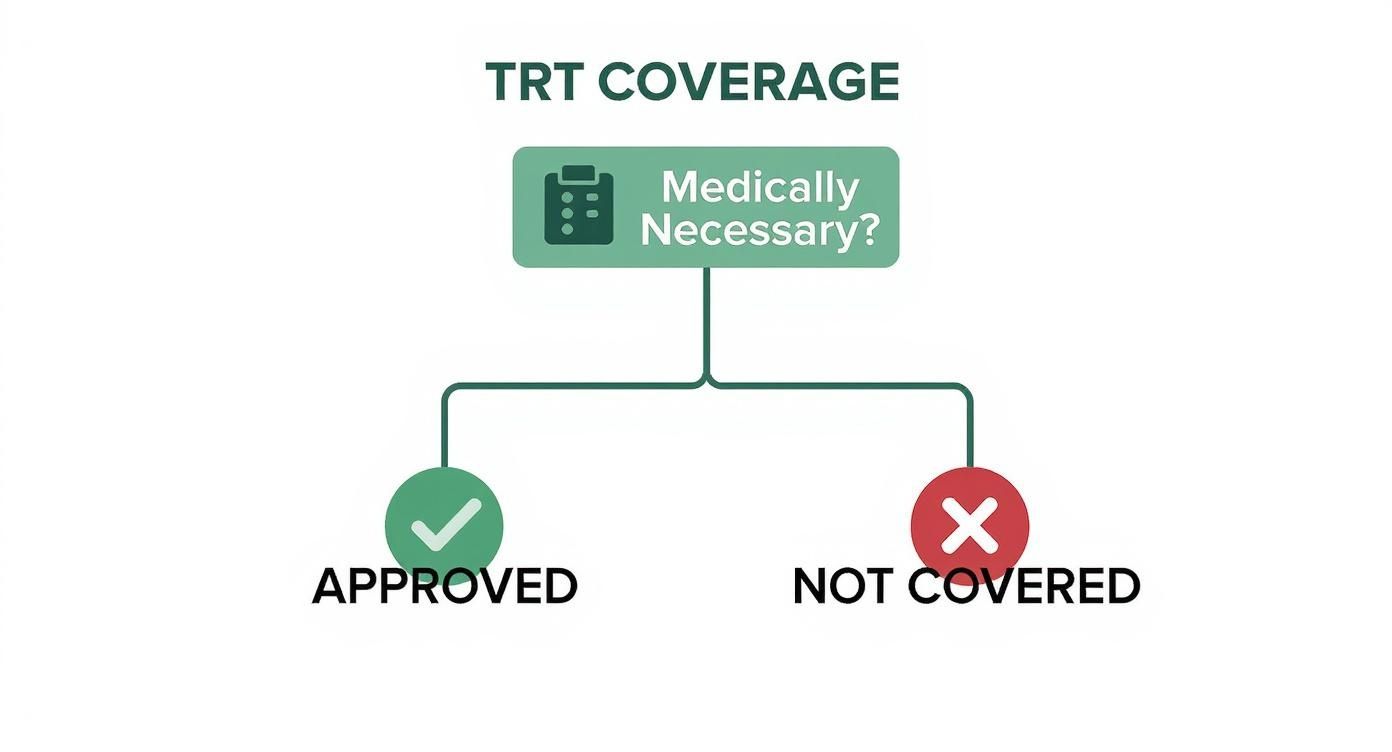
Ultimately, getting a "yes" on medical necessity leads straight to approval, while a "no" results in a denial. It’s why having solid proof is completely non-negotiable. Your claim has to scream "medical need," not just a desire for optimization.
Gathering the Right Paperwork for Approval
Successfully getting your TRT covered by insurance is less about the prescription itself and more about the mountain of paperwork you can build to back it up. Think of it like you're building a case for a judge. Just asking for approval isn't enough—you need to hand them a file so packed with solid evidence that they have no choice but to say yes.
Make no mistake, your insurance provider will scrutinize every single page. This means you and your doctor need to be on the same team, meticulously putting together a complete narrative that proves this treatment is a medical necessity, not just a preference. A simple prescription slip is just the opening line in this conversation.
Your Documentation Checklist
To build a claim that sails through the approval process, your submission package has to be airtight. Every document plays a specific role, working together to paint a clear picture of your diagnosis and why TRT is the right call.
Here’s what you absolutely must have:
- Certified Lab Results: This isn't a one-and-done deal. You need at least two separate, early-morning blood tests showing your testosterone is consistently below the insurer’s threshold, which is typically under 300 ng/dL.
- Physician’s Chart Notes: These are gold. Your doctor's notes create a timeline of your symptoms—fatigue, low libido, brain fog—and directly connect them to your low testosterone levels. It's the story of your struggle in black and white.
- The Letter of Medical Necessity: This is the centerpiece of your entire claim. Your doctor writes this letter to formally explain your situation to the insurer in a language they understand.
The letter has to be crystal clear. It must state your official diagnosis of hypogonadism, explain why other treatments aren't a good fit, and detail exactly how TRT is expected to resolve your specific medical symptoms.
Working closely with your healthcare provider is key. For those looking to make this process as smooth as possible, an online doctor consultation can be a huge help in ensuring all your paperwork is perfectly aligned with what insurers are looking for. When your submission is well-organized and undeniable, a denial becomes far less likely.
How Insurance Views Different Types of TRT
When it comes to getting your TRT covered by insurance, not all treatment methods are seen as equal. The decision often boils down to one simple factor: cost. Insurers will almost always steer you toward the most cost-effective, proven option first.
Think of it as a tiered system. Generic, injectable testosterone is the foundation—the most affordable and established treatment. Because it has a long history of getting the job done reliably and inexpensively, it’s the method insurance companies are most willing to approve without a fight.
However, more modern or convenient options—like daily gels, patches, or long-lasting pellets—are viewed with a lot more suspicion. These are often brand-name treatments and are significantly more expensive, so insurers put up higher barriers before they'll agree to pay.
Understanding Step Therapy and Prior Authorization
To keep costs down on these pricier options, insurers use two key strategies: step therapy and prior authorization. Getting a handle on these terms is crucial if you're trying to navigate TRT coverage.
- Step Therapy: This is basically a "try the cheapest first" rule. Your insurance plan will likely require you to try—and "fail"—with generic testosterone injections before they will even consider covering a more expensive gel or patch. You have to prove the lower-cost option didn’t work for you.
- Prior Authorization: For any TRT method that isn't their preferred choice, your doctor has to send in extra paperwork justifying why you need that specific treatment. They have to build a strong case that the more expensive option is medically necessary, not just a matter of convenience.
Even with progress, coverage is far from guaranteed. Only about 65% of U.S. private health plans cover TRT for classic hypogonadism. Coverage through Medicare and Medicaid can be even more inconsistent, often tied to very strict diagnostic criteria. You can learn more about the complexities of TRT insurance coverage and market trends to better understand these variations.
The takeaway is simple: your insurer’s goal is to manage costs. They will almost always push you and your doctor toward the most economical treatment path, which usually starts with injections.
This reality makes it critical to have an open conversation with your doctor about all available TRT methods. Knowing where your insurer likely stands helps you set realistic expectations and map out the best strategy for getting covered.
Comparing Insurance Coverage By TRT Method
Your choice of TRT method directly impacts how your insurance company will approach coverage. In their eyes, it's a simple calculation of cost versus necessity. The table below breaks down the most common TRT delivery methods, their typical out-of-pocket costs, and what you can generally expect from your insurance provider.
| TRT Method | Average Cost (Without Insurance) | Typical Insurance Coverage | Common Requirements |
|---|---|---|---|
| Injections | $40 – $100 per month | Most Likely to be Covered | Often the first-line treatment. May require a confirmed diagnosis of hypogonadism. |
| Gels/Creams | $500 – $800 per month | Coverage is Possible | Almost always requires prior authorization and failure of injections first (step therapy). |
| Patches | $500 – $700 per month | Coverage is Possible | Similar to gels; requires prior authorization and proof that injections were not effective. |
| Pellets | $600 – $1,200 per procedure | Least Likely to be Covered | Often considered elective or a "convenience" item. Very difficult to get approved. |
As you can see, the financial path of least resistance for an insurer always points back to injections. While gels, patches, and pellets offer convenience, you and your doctor will have to be prepared to document exactly why these more expensive options are medically essential for your specific situation. Your doctor's role in navigating the paperwork for prior authorizations is key.
What to Do When Your TRT Claim Is Denied

Getting that denial letter for your TRT claim feels like hitting a brick wall. But here's the reality: it’s rarely the final word. Think of it as the insurance company’s opening move in a negotiation, not a checkmate.
Most of these initial denials are automated. A computer algorithm likely flagged something—maybe a piece of missing information or a lab value that was just a hair outside the required range. The first step is to see that letter not as a rejection, but as your roadmap. It tells you exactly why they said no, which is the key to planning your next move.
Crafting Your Appeal Strategy
Once you know the "why," you and your doctor can put together a targeted appeal. Just resubmitting the same paperwork and hoping for a different outcome is a waste of time. You need to address the specific reason for the denial head-on. A strong appeal is always a team effort between you and your healthcare provider.
Your game plan should look something like this:
- Analyze the Denial Reason: Did they claim your testosterone wasn't low enough? Was a specific document missing? Get crystal clear on the exact problem.
- Gather New Evidence: If the denial was because of a borderline lab result, your doctor might order another early-morning blood test to get a more accurate reading. If they needed more proof of symptoms, your doctor can add more detailed clinical notes to your file.
- Draft a Compelling Appeal Letter: Your doctor needs to write a formal letter that directly counters the insurer's reason for denial. This letter should reinforce your diagnosis, stress the medical necessity of TRT for your health, and include any new evidence you've gathered.
A classic reason for denial is a borderline testosterone level—say, 305 ng/dL when the insurance cutoff is 300 ng/dL. In cases like this, getting additional testing done is your single strongest weapon for a successful appeal.
Understanding the Appeals Process
If your first appeal gets rejected, you're not out of options. Most insurance plans have a multi-level appeals process. The first round is an internal appeal, where you’re essentially asking the insurance company to have a different person take a second look at your case.
If that doesn't work, you can request an external review. This is where the real power lies. An independent, third-party doctor with no ties to your insurer reviews all the evidence. Their decision is usually binding. Just knowing these next steps exist can give you the confidence to keep fighting for the coverage you need.
Your Top Questions About TRT and Insurance, Answered
Let's be honest: trying to understand insurance policies can feel like decoding a secret language. Even when you think you have the main rules down, specific situations always bring up more questions. Here are the straight-up answers to the most common hurdles people face when getting insurance to pay for TRT.
Will My Insurance Cover an Online TRT Clinic?
This is a tricky one. While telehealth has become a normal part of healthcare, many insurance companies are still old-school and have strict rules about in-network doctors. Some insurers are flat-out skeptical of a diagnosis that doesn't come from a traditional, face-to-face physical exam.
Before you sign up with any online provider, you need to call your insurance company and get two very direct questions answered: "Is this specific online clinic in my network?" and "Do you accept their process for diagnosing low testosterone?" Getting a clear "yes" on both is the only real way to protect yourself from getting stuck with the entire bill.
Does Medicare Cover Testosterone Replacement Therapy?
Yes, but expect a tough road ahead. Medicare Part B and Part D can cover TRT, but their rules are incredibly rigid. They will only consider it for hypogonadism caused by specific, well-documented medical problems like testicular failure or pituitary gland disorders.
The key takeaway here is that Medicare will not cover TRT for symptoms tied to the natural decline of testosterone that comes with age. You have to hit their exact low-T lab numbers, and your doctor must provide a mountain of paperwork proving it's a medical necessity. Even then, your standard deductibles and co-pays will still apply.
What Happens if My Testosterone Levels Are Borderline?
This is probably the single most common reason for an initial denial. If your lab work comes back just a hair above the insurer’s cutoff—say, 310 ng/dL when their policy requires 300 ng/dL—the claim will almost certainly be rejected by their automated system. It doesn't matter how severe your symptoms are.
In this situation, your doctor’s best move is to order more morning blood tests. Testosterone levels change throughout the day and are always highest in the morning, so a test on another day could easily dip below that magic number. A powerfully written letter of appeal from your doctor can help, but it’s far more likely to succeed when it's backed by lab results that clearly tick the insurer's box.
Will Insurance Also Pay for My Follow-Up Blood Work?
For the most part, yes. If your insurance company approves your TRT as medically necessary, they will almost always cover the monitoring that goes with it. This includes the follow-up blood tests you need to check your hormone levels, hematocrit, and other important health markers.
Your regular doctor's visits to manage the treatment are also typically covered since they're all considered part of the standard of care for TRT. Just remember, these services will still be subject to your plan’s normal co-pays, co-insurance, and deductibles, just like any other lab work or appointment.
At Elite Bioscience, we help you navigate your health goals with clarity and confidence. Our streamlined process provides access to premium therapies designed for your wellness journey. Take control of your health today by visiting us at https://elitebioscience.co.
QUICK SEARCH
Make an account today to start your journey towards a better and healthier lifestyle.