What Is Hormone Replacement Therapy? Discover Key Facts & Benefits
So, what exactly is hormone replacement therapy (HRT)? At its core, it's a medical treatment that gives back the hormones your body isn't making enough of anymore, most often during menopause.
Think of your body's hormonal system as a finely tuned internal thermostat. When hormones like estrogen and progesterone start to decline, that thermostat can go haywire. The result? Unpredictable and disruptive symptoms like hot flashes, night sweats, and mood swings. HRT works by stabilizing that internal control system, restoring balance to relieve those symptoms and improve your overall quality of life.
The Growing Demand for Hormonal Balance
The need for this kind of hormonal support is becoming more widely recognized. The global market for hormone replacement therapy was valued at around $24.26 billion in 2024 and is expected to climb to $46.32 billion by 2034. This isn't just a trend; it reflects a growing awareness of menopausal health and the therapy's ability to help manage a range of hormonal conditions. You can see more details about this trend in the full market analysis.
Core Concepts of HRT
To really get a handle on what hormone replacement therapy is, it's helpful to understand its fundamental principles. This isn't a one-size-fits-all pill. It's a personalized medical strategy designed around your specific symptoms and health needs.
The main objectives of HRT are twofold: to improve your immediate quality of life by managing symptoms and to help reduce the long-term risk of certain degenerative diseases associated with aging, like osteoporosis.
This dual focus on both present comfort and future health is what makes HRT such a cornerstone of care for so many people. While traditional HRT is very common, many individuals are also exploring options like bioidentical hormone replacement therapy to find a solution that feels perfectly aligned with their body's unique chemistry.
To break it down even further, here's a quick look at the key concepts of HRT at a glance.
HRT at a Glance Key Concepts
This table summarizes the foundational aspects of Hormone Replacement Therapy, offering a clear and quick overview for better understanding.
| Concept | Brief Explanation |
|---|---|
| Primary Goal | To relieve moderate to severe symptoms of menopause by replenishing declining hormone levels. |
| Key Hormones | Estrogen is the primary hormone for symptom relief. Progesterone is added to protect the uterus in women who still have one. |
| Personalization | Treatment is tailored to individual needs, using the lowest effective dose for the shortest necessary time. |
| Delivery Methods | Can be administered via pills, patches, gels, creams, or rings, depending on symptoms and personal preference. |
| Dual Benefit | Aims to improve current quality of life (symptom relief) and support long-term health (e.g., bone density). |
As you can see, the approach is highly individualized and designed with both immediate and future health in mind.
There are several key components to consider when discussing HRT with a provider:
- Hormones Used: The most common are estrogen and progesterone. Estrogen is the workhorse for relieving symptoms like hot flashes, while progesterone is added to protect the uterine lining.
- Delivery Methods: HRT isn't just a pill. It can be delivered through skin patches, gels, creams, or vaginal rings. The method you choose often depends on your specific symptoms and what works best for your lifestyle.
- Treatment Goals: The modern approach is all about precision. The goal is to use the lowest effective dose for the shortest duration necessary to get you feeling better, all while minimizing any potential risks.
Exploring the Different Types of HRT
When we talk about hormone replacement therapy (HRT), it’s crucial to understand it’s not a one-size-fits-all pill. HRT is a highly personalized medical strategy. Think of it less like a standard prescription you pick up at the pharmacy and more like a custom-tailored suit, designed to fit your unique body, symptoms, and health profile perfectly.
The first major choice you and your doctor will make is between systemic and local therapy. This decision comes down to what symptoms you're trying to solve.
Systemic Hormone Therapy
Systemic HRT is designed to work throughout your entire body. The hormones enter your bloodstream and travel everywhere, making this approach ideal for tackling the widespread symptoms of menopause—the kind that affect you from head to toe. We're talking about hot flashes, night sweats, mood swings, and that frustrating brain fog.
Because the hormones circulate everywhere, they can act on all the different tissues that need them, providing comprehensive relief.
There are several ways to get systemic HRT, each with its own pros and cons to consider:
- Oral Pills: This is the most traditional method. You simply take a pill every day to maintain a steady level of hormones.
- Skin Patches: These are applied to the skin (usually on your abdomen or buttocks) and you change them every few days. This method is great because it bypasses the liver, which can be an advantage for some people.
- Topical Gels or Sprays: You apply these to your skin daily, allowing the hormones to absorb directly into your bloodstream.
This infographic gives you a quick visual breakdown of the different ways HRT can be delivered.
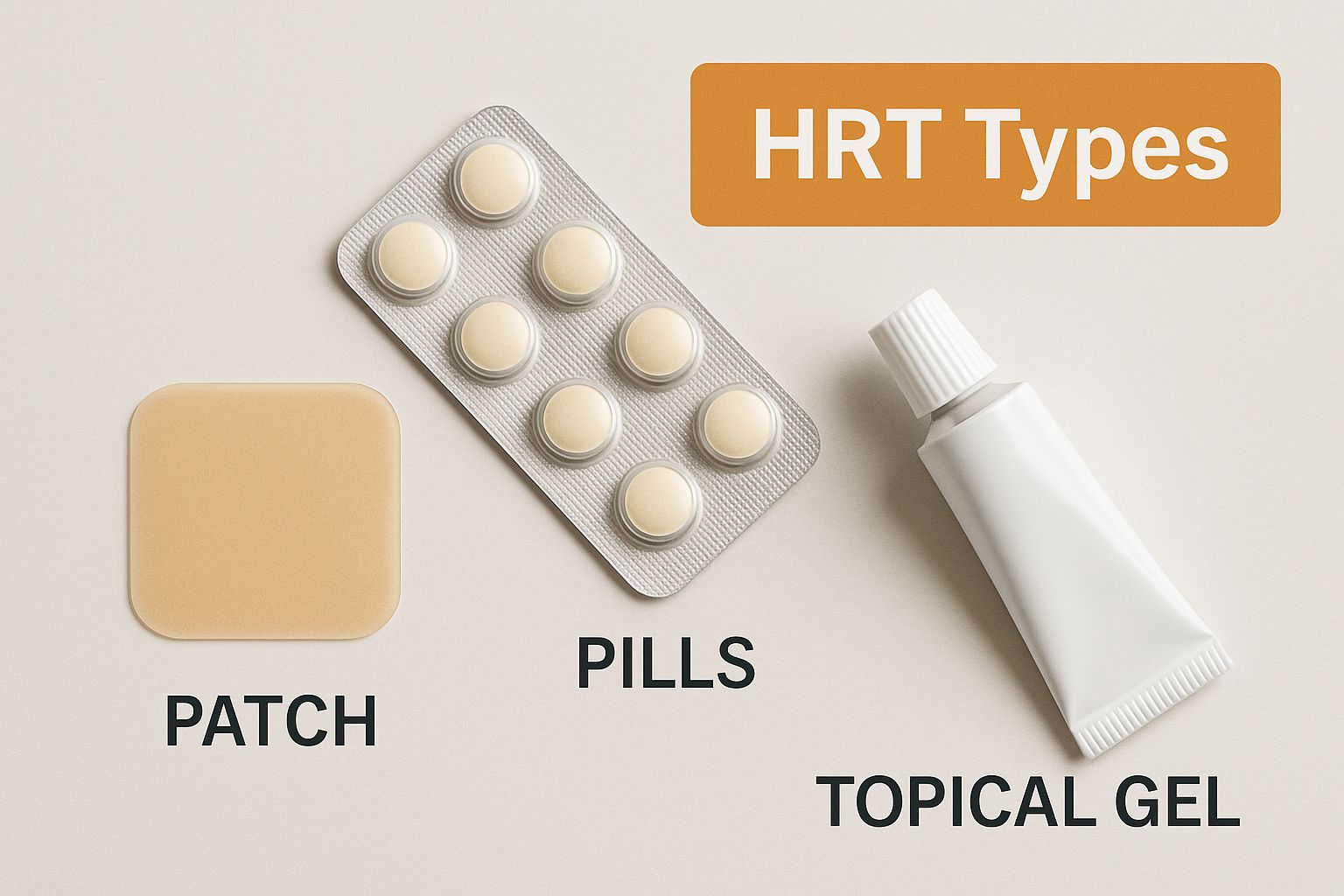
The sheer variety of options, from patches to gels, really shows how treatment can be adapted to fit different lifestyles and medical needs.
Local Hormone Therapy
In contrast, local hormone therapy is all about targeting a specific area. It’s an excellent choice if your symptoms are concentrated in one place, most commonly for vaginal dryness, pain during sex, or urinary issues.
Local therapies use a very low dose and are designed to work only where you apply them. This means there's minimal absorption into the rest of the body, which is a big plus because it minimizes your overall exposure to hormones.
Common forms of local HRT include:
- Vaginal Creams: You apply these directly inside the vagina using an applicator.
- Vaginal Tablets: A small, dissolvable tablet that you insert into the vagina.
- Vaginal Rings: This is a flexible ring that you place inside your vagina, where it slowly releases hormones over several months.
Hormone Combinations Used in HRT
Beyond how you take it, what hormones you take is the other critical piece of your personalized plan. This decision is based almost entirely on one simple question: do you have a uterus?
Estrogen-Only Therapy (ET):
If you've had a hysterectomy (surgery to remove your uterus), your doctor will most likely prescribe estrogen by itself. Estrogen is the main hormone that relieves most menopausal symptoms. Since you don't have a uterus, there's no need for progestin to protect it.
Combination Therapy (EPT):
If you still have your uterus, you will be prescribed a combination of estrogen plus progestin (a synthetic version of progesterone). This is incredibly important. Taking estrogen alone can cause the lining of the uterus (the endometrium) to build up, which increases the risk of endometrial cancer. Progestin is added specifically to balance estrogen’s effects and keep that lining thin, protecting your uterus.
This careful, tailored approach reflects how much more sophisticated menopausal healthcare has become. This growing awareness is also fueling major market growth. The global HRT market is projected to hit around $18.99 billion in 2025 and is expected to climb to approximately $33.69 billion by 2035. You can find more data about this expansion and its drivers in the full market insights.
Ultimately, choosing the right type of HRT is a collaborative decision between you and your healthcare provider, ensuring your treatment plan is safe, effective, and perfectly aligned with your health goals.
The Real-World Benefits of Undergoing HRT
Medical definitions are one thing, but understanding what hormone replacement therapy is really clicks when you see the difference it makes in someone’s everyday life. For many people, HRT isn't just about topping up hormone levels; it's about getting back a sense of who they are—the energy and stability that menopause can quietly take away. The impact is often profound, covering everything from quick symptom relief to safeguarding your health for years to come.

The most celebrated benefit is how it handles vasomotor symptoms. That’s the clinical term for those sudden, intense hot flashes and drenching night sweats that can completely disrupt your day and ruin your sleep. By bringing estrogen levels back into balance, HRT essentially calms down the body’s haywire internal thermostat.
Immediate Improvements in Daily Life
One of the first changes people usually report is a huge drop in these frustrating symptoms. In fact, research shows that estrogen therapy is still the single most effective treatment for hot flashes, cutting their frequency by about 75% and their severity even more.
This relief creates a powerful ripple effect that improves your entire quality of life:
- Better Sleep: Fewer night sweats mean you’re not waking up constantly. Getting consistent, deep sleep is the foundation for a good mood, sharp thinking, and daytime energy.
- Stable Moods: The hormonal roller coaster of menopause is famous for causing irritability, anxiety, and sudden waves of sadness. HRT helps smooth out those hormonal peaks and valleys, leading to a much more balanced and positive emotional state.
- Enhanced Mental Clarity: So many people talk about lifting the frustrating "brain fog" that comes with menopause. With HRT, they often find their focus and concentration return.
The core objective is not just to manage symptoms, but to improve your present quality of life while simultaneously investing in your future health. This dual focus is what makes HRT a cornerstone of modern menopausal care.
Hormone therapy isn't limited to just estrogen and progesterone. For some, other hormones are key to feeling their best. You can explore the surprising benefits of testosterone therapy for women, which can be another piece of the puzzle for restoring energy and vitality.
Crucial Long-Term Health Advantages
While getting rid of hot flashes is a huge win, the long-term protective benefits of HRT are just as important. Think of it as a forward-thinking strategy for your future, helping to defend against health issues that become more common after menopause.
One of the most significant long-term advantages is protection against osteoporosis. This is a condition where bones become weak and brittle, leaving you much more vulnerable to fractures.
Estrogen is vital for keeping bones strong. When its levels plummet during menopause, bone loss can speed up dramatically. By replenishing estrogen, HRT helps slow this process way down, significantly reducing the risk of a debilitating hip, spine, or wrist fracture later in life.
On top of that, HRT can offer cardiovascular protection for many women. When started in women under 60 or within 10 years of menopause, studies show it can lower the risk of heart disease and improve overall longevity by helping to keep blood vessels flexible and manage cholesterol levels.
In the end, all these benefits come together to do more than just provide physical relief. They give you a renewed sense of control and help you feel more like yourself again—energetic, clear-headed, and ready to live life to the fullest.
Navigating The Potential Risks And Side Effects
Any real conversation about hormone replacement therapy needs an honest look at the potential downsides. Let's be clear: every effective medical treatment has potential risks and side effects, and HRT is no exception. The goal isn't to be scared of them, but to understand them in the context of your own health so you can make a clear-eyed, informed decision.

A lot of the public fear around HRT comes from a major study back in the early 2000s, the Women's Health Initiative (WHI). Its initial findings painted a scary picture, highlighting increased risks that caused a great deal of alarm. But medicine has come a long way since then. A closer look at that same WHI data, plus years of newer studies, has given us a much more nuanced view. We now know the risks aren't universal; they depend heavily on a few key factors.
Understanding The Major Risk Factors
The level of risk with HRT isn't the same for everyone. It’s more like a sliding scale that shifts based on your personal health profile. Modern medicine is all about personalizing treatment to keep these risks as low as possible, and that starts with your age, the type of HRT you use, and your treatment timeline.
Here are the main risk factors we consider:
- Age and Timing: This is probably the most critical piece of the puzzle. For women who start HRT under the age of 60 or within 10 years of their last period, the benefits very often outweigh the risks. The potential for risk tends to climb for women who start therapy later in life.
- Type of HRT: The specific hormones matter. Combination therapy (estrogen plus progestin) has been linked to a slightly higher risk of breast cancer than estrogen-only therapy.
- Duration of Use: The longer you're on HRT, some risks, like breast cancer, can increase. This is precisely why the standard approach is to use the lowest effective dose for the shortest amount of time necessary to manage your symptoms.
- Personal Health History: Your own medical story and your family's history are hugely important. A personal history of breast cancer, ovarian cancer, blood clots, heart disease, or stroke would make HRT a much riskier choice.
A Closer Look At Serious Health Concerns
When we talk about risks, the conversation usually turns to the most serious concerns: blood clots and certain cancers. It’s important to put these risks in perspective. For example, while oral HRT does increase the risk of blood clots, the absolute risk for most healthy women is still very low. Switching to a transdermal patch or gel can lower this risk even further because the hormones bypass the liver.
This careful risk assessment is why medical supervision is non-negotiable. While the market for hormone replacement therapy shows strong growth, this is balanced by a healthy caution around long-term use. Concerns about increased risks of blood clots, heart attacks, and breast cancer with prolonged therapy mean that every patient needs a thorough, individual risk evaluation.
The modern approach to HRT isn't about avoiding risk altogether—that's impossible. It's about managing it intelligently. A deep conversation with your doctor is the only way to evaluate your personal risk profile and create a plan that’s both safe and effective for you.
For a more detailed look, you can read our complete guide on hormone replacement therapy side effects.
Managing Common, Less Severe Side Effects
Beyond the major health risks, it's pretty common for people to experience milder, temporary side effects when they first start HRT. Think of it as an adjustment period for your body as it gets used to new hormone levels. These issues usually go away on their own within a few months as your system finds its new equilibrium.
Some common, temporary side effects include:
- Fluid Retention and Bloating: Often one of the first things people notice, but it typically settles down.
- Breast Tenderness or Swelling: This is a common reaction to estrogen, similar to what you might feel during a menstrual cycle.
- Headaches or Migraines: For some, HRT can be a trigger. For others, it actually makes them better. It's very individual.
- Mood Swings or Irritability: While HRT often helps stabilize mood in the long run, you might experience some fluctuations as your body adapts.
- Nausea: This can sometimes happen with oral estrogen, but taking it with food often helps.
If these side effects stick around, it doesn't mean HRT isn't for you. Often, a simple tweak to your dose, the type of hormone, or how you take it (like switching from a pill to a patch) can solve the problem. This is exactly why regular follow-up appointments with your provider are a critical part of the process—they ensure your HRT journey is as smooth and helpful as possible.
Determining If You Are a Good Candidate for HRT
Deciding if hormone replacement therapy is the right move for you is a deeply personal journey, and it always starts with an honest conversation with your healthcare provider. It’s not a simple yes-or-no question. Instead, it’s a careful evaluation of your symptoms, your age, your unique health history, and what you want for your long-term well-being.
The core question we always have to answer is this: do the potential benefits of HRT outweigh the potential risks for you? Your provider is your guide in this process, helping you weigh all the factors so you can confidently decide whether to explore this treatment any further.
Who Is an Ideal Candidate for HRT?
While every woman's situation is unique, medical guidelines have helped us pinpoint a "sweet spot" where HRT tends to be most beneficial with the lowest risk. The ideal candidate for starting hormone therapy is usually someone who fits a specific profile based on their age and how symptoms are affecting their life.
Typically, an ideal candidate is:
- Under 60 years old: Research has consistently shown that starting therapy before age 60 is generally safer.
- Within 10 years of menopause: Timing is everything. Beginning HRT within a decade of your last period is linked to the best balance of benefits to risks.
- Experiencing disruptive symptoms: The main reason to start HRT is to get relief from moderate to severe menopausal symptoms—like hot flashes, night sweats, or vaginal dryness—that are actively getting in the way of your quality of life.
Think of this as a window of opportunity. For many women in their 40s and 50s, starting HRT during this timeframe can provide maximum symptom relief while keeping potential risks at their lowest.
This targeted approach helps ensure that the people who stand to gain the most from what hormone replacement therapy is are the ones who receive it.
When HRT Is Usually Not Recommended
Just as important as knowing who is a good candidate is understanding who is not. Certain medical conditions, which we call contraindications, make the risks of HRT simply too high. Your doctor will do a thorough review of your medical history to spot any of these red flags.
HRT is generally not recommended if you have a personal history of:
- Breast Cancer: A past diagnosis of estrogen-sensitive breast cancer is a major reason to avoid HRT.
- Other Cancers: A history of certain other hormone-sensitive cancers, like ovarian or uterine (endometrial) cancer.
- Blood Clots: Previous episodes of deep vein thrombosis (DVT) or a pulmonary embolism.
- Stroke or Heart Attack: A past stroke or heart attack significantly raises the risk profile.
- Unexplained Vaginal Bleeding: This always needs to be fully investigated before even considering hormone therapy.
- Certain Liver Diseases: Because some forms of HRT are processed by the liver, a history of liver disease is a key factor.
Your family’s medical history can also play a role in this decision. The entire goal is to get a complete, 360-degree view of your personal health landscape. This careful, personalized medical evaluation is the cornerstone of any successful and safe HRT journey.
Your HRT Journey From First Talk to Treatment
Taking the first step toward hormone replacement therapy can feel like a big deal, but knowing what the process looks like can make it far less intimidating. Your journey with HRT isn't a one-time event; it's a collaborative path you walk with your healthcare provider, starting with a simple, honest conversation about what you're going through.
Your first appointment is all about telling your story. Be ready to talk openly about your symptoms—and not just the hot flashes. Think about changes in your sleep, your mood, your energy levels, and how you feel day-to-day. This conversation is essential because it gives your provider a real-world picture of how menopause is affecting your life.
The Initial Consultation and Evaluation
To get the full picture, your doctor will need to do a thorough evaluation. This usually starts with a deep dive into your personal and family medical history. They’ll want to know about any past health conditions, especially any that might make HRT a riskier choice for you.
Based on that discussion, your provider will likely suggest a few key tests to gather more information. These typically include:
- Blood Tests: To check your hormone levels (like estrogen and follicle-stimulating hormone, or FSH) and get a clear baseline. This helps confirm whether you're in perimenopause or menopause.
- Physical Exam: This will include a pelvic exam and a blood pressure check to make sure you're in good health to start therapy.
- Mammogram: An important step to check your breast health before you begin any hormone treatment.
This evaluation stage is all about gathering information. Think of it like a detective building a case file—your doctor is collecting all the clues needed to determine if HRT is a safe and effective option for you.
Once all this information is on the table, you and your provider will go over the results together. If you’re a good candidate, the conversation will shift toward creating a personalized treatment plan designed around your specific symptoms and health profile.
Starting Treatment and Finding Your Balance
With a solid plan in hand, the next step is to actually begin the treatment. This is where we bring in the different delivery methods we talked about earlier—like pills, patches, or gels. Your provider will help you select the one that fits best with your lifestyle and medical needs.
The first few weeks and months are really an adjustment period. Your body needs time to get used to the new hormone levels, so don't expect perfection overnight. It's important to remember that the first prescription isn't always the final one. Finding the perfect dose and type of HRT often takes a little fine-tuning.
This is why ongoing care is a non-negotiable part of the journey. You'll have follow-up appointments, usually about three months after you start and then annually after that. These check-ins are absolutely vital for:
- Monitoring Your Progress: Talking about how your symptoms are changing and, most importantly, how you're feeling.
- Adjusting Your Dosage: Making small tweaks to your prescription to maximize the benefits and keep any side effects to a minimum.
- Ensuring Safety: Performing routine health checks to make sure the therapy continues to be a safe choice for you.
This continuous partnership ensures your HRT journey is effective, safe, and perfectly aligned with your health goals every step of the way.
Of course, here is the rewritten section, crafted to match the expert, human-written style of the provided examples.
Your HRT Questions, Answered
As you get closer to making a decision about hormone replacement therapy, it's completely normal for specific, practical questions to surface. This is where the big-picture concepts meet real-world application. Let's tackle some of the most common concerns we hear, clearing up any lingering confusion so you can move forward with confidence.
How Long Can I Safely Take HRT?
This is probably the most frequent question we get, and the answer has changed a lot over the years. We've moved away from the old, rigid idea that there's a universal "end date" for everyone. The modern medical approach is to use the lowest effective dose for the shortest amount of time necessary to manage your symptoms.
For many women, this ends up being about five years, but that’s just an average, not a rule. Think of your HRT plan as a dynamic partnership with your doctor. You'll regularly check in, re-evaluating the benefits versus any potential risks as your body and health needs continue to evolve.
Does HRT Cause Weight Gain?
This is a huge worry for many women, but the research is pretty clear: HRT itself isn't the culprit behind menopausal weight gain. The body changes often blamed on the therapy are actually driven by the natural hormonal shifts of menopause itself.
Menopause can slow your metabolism and change how your body stores fat, often leading to more accumulation around your midsection. Some women on HRT actually find it easier to manage their weight because their other symptoms, like poor sleep and low energy, finally improve.
By getting your hormones back in balance, HRT can restore the energy and stability you need to stick with a healthy lifestyle—which is the real key to managing your weight during this stage of life.
What Are Bioidentical Hormones?
The term "bioidentical" sounds incredibly natural and appealing, but it's important to know what it actually means. Bioidentical hormones are simply hormones that are chemically identical on a molecular level to the ones your own body produces. They are often derived from plant sources.
It's crucial, however, to understand the two main forms they come in:
- FDA-Approved Products: Many standard, conventional HRT prescriptions you'd get from any pharmacy are already bioidentical. These have been rigorously tested for safety and efficacy.
- Custom-Compounded Formulas (cBHRT): These are custom-mixed at special compounding pharmacies based on a doctor's specific recipe for an individual patient.
While the idea of a "custom mix" sounds ideal, it's vital to know that custom-compounded versions are not regulated by the FDA for safety, purity, or effectiveness in the same way standard prescriptions are. This is a critical point to discuss with your provider when you're exploring all your treatment options.
At Elite Bioscience, we believe clear, medically sound information is the foundation of empowered health decisions. Our team specializes in hormone therapies designed to fit your unique physiology, with an unwavering focus on safety, quality, and convenience. To learn more about how we can support your wellness journey, explore our personalized treatments.
QUICK SEARCH
Make an account today to start your journey towards a better and healthier lifestyle.