When you start Hormone Replacement Therapy (HRT), it’s a bit like recalibrating your body's internal thermostat. It’s completely normal for there to be an adjustment period as your system gets used to the new hormone levels. While HRT can be a game-changer for managing difficult menopause symptoms, it's smart to be both curious and cautious about the potential side effects.
This guide is designed to be a clear, straightforward starting point for an informed conversation with your doctor. We’ll walk through the common, temporary changes you might notice and the less frequent but more serious risks you need to be aware of. Understanding this difference is key to feeling prepared and confident as you begin treatment.
Common vs. Serious Side Effects
It's helpful to sort side effects into two main buckets: the initial "getting to know you" phase and the more significant health considerations.
- Initial Adjustment Effects: These are usually mild and temporary. Think of them as your body figuring things out with the new hormone levels. This can include things like bloating, moodiness, or breast tenderness.
- Serious Health Risks: These are much less common but require a careful conversation with your doctor. This category includes risks like blood clots, which are influenced by the type of HRT you use and your personal health history.
For most women, the relief from disruptive symptoms like hot flashes and night sweats far outweighs these initial hurdles.
The goal of modern hormone therapy is to use the lowest effective dose for the shortest necessary time to manage symptoms while minimizing risks. This personalized approach ensures your treatment plan is tailored specifically to your body's needs and health profile.
To give you a clearer picture of what to expect in the first few months, the table below summarizes the most common side effects, when they typically show up, and how long they usually stick around.
Common HRT Side Effects and Typical Onset
| Side Effect | Typical Onset | Notes and Duration |
|---|---|---|
| Breast Tenderness | 1-4 weeks | Often feels similar to premenstrual tenderness and usually subsides within 3 months as your body adjusts. |
| Bloating & Fluid Retention | 1-2 weeks | Caused by estrogen's effect on fluid balance; typically improves with dietary adjustments and time. |
| Nausea | 1-3 weeks | More common with oral HRT. Taking it with food or switching to a patch or gel can often resolve this. |
| Headaches | 2-6 weeks | Hormonal fluctuations can trigger headaches. These often lessen as your hormone levels stabilize. |
This table helps set realistic expectations for the initial adjustment period.
For those wanting to explore different formulations, learning about bioidentical hormone replacement therapy can provide more insight into highly personalized options. Remember, your journey is unique, and being well-informed is the best first step toward finding the right balance for your health.
The Initial Adjustment: Common HRT Side Effects

Starting Hormone Replacement Therapy (HRT) is a bit like turning up the thermostat in a house that’s been chilly for a long time. Your body has been operating at a certain “hormonal temperature” for years, and now you’re asking it to recalibrate to a new normal. This adjustment period is precisely why many women experience temporary and mild hormone replacement therapy side effects during the first few weeks or months.
These early symptoms are almost never a sign that something is wrong. Instead, they’re just your body getting acquainted with new levels of estrogen and, in some cases, progestin. Most of these effects are completely manageable and tend to fade away as your system finds its new balance. Knowing what to expect can make this transition feel much less intimidating.
Understanding Common Physical Adjustments
Some of the most frequently reported side effects are physical discomforts that pop up as your body responds to the reintroduction of hormones. It’s a completely normal part of the process.
Bloating and Fluid Retention
Feeling puffy or bloated is a classic example. Estrogen can influence how your body manages salt and water, which sometimes leads to temporary fluid retention. This is usually most noticeable in the first month and almost always resolves on its own.
Breast Tenderness
If you’ve ever had sore breasts before your period, this sensation might feel familiar. The new hormones can stimulate breast tissue, causing some tenderness or swelling. For most women, this discomfort is temporary and settles down within three months.
Nausea
Some women report feeling a bit queasy, especially when taking oral estrogen. This side effect is often tied to the hormone dose making its way through your digestive system.
Think of it as a temporary conversation between the new hormones and your body. At first, the signals can get a little crossed, leading to these minor issues. With time, the communication smooths out, and the side effects often disappear.
Navigating Mood and Other Symptoms
Hormones don't just affect us physically; they are powerful regulators of our mood and overall sense of well-being.
Mood Swings
Just like the hormonal dips of perimenopause can cause irritability or sadness, introducing new hormones can temporarily stir the pot. Your brain needs time to adjust to these new signals, which can lead to fleeting mood changes as it finds its new equilibrium.
Headaches
Hormonal fluctuations are a well-known trigger for headaches. When you start HRT, the change in your estrogen levels can sometimes bring on temporary headaches or migraines, especially if you were already prone to them.
Practical Tips for Managing Initial Side Effects
The good news is that you don't just have to ride it out. There are simple, practical steps you can take to manage these common hormone replacement therapy side effects and make the transition feel smoother.
- For Bloating: Try cutting back on salt, drinking plenty of water, and adding potassium-rich foods like bananas and avocados. This can help your body flush out excess fluid more efficiently.
- For Nausea: If you’re taking HRT pills, try having them with a meal or a small snack. If the nausea sticks around, talk to your doctor about switching to a transdermal option like a patch or gel, which bypasses the digestive system altogether.
- For Breast Tenderness: A supportive, well-fitting bra can make a world of difference. Some women also find that avoiding caffeine and reducing salt can help provide relief.
- For Headaches: Make sure you are well-hydrated and keeping a consistent sleep schedule. If headaches are a problem, discuss the timing and dosage with your doctor—a small tweak can often resolve the issue.
These early side effects are a normal rite of passage for many. By staying in close communication with your healthcare provider, you can make small adjustments to your routine or treatment plan to make sure you stay comfortable as your body adapts.
Understanding the Major Health Risks of HRT
While the initial bumps in the road with HRT are usually temporary, we need to have a frank discussion about the more serious health risks. It’s crucial to approach this with facts, not fear. For years, the conversation around hormone therapy was driven by scary headlines that left out critical details, making countless women anxious and confused about their options.
Let's get one thing straight: understanding these risks isn't about scaring you away from treatment. It's about giving you a clear, balanced perspective so you can walk into your doctor's office feeling empowered. This knowledge is what allows you to have a productive, collaborative conversation about whether HRT is a good fit for you.
The Landmark Study That Changed Everything
So much of what we know today about the major risks of HRT comes from one groundbreaking piece of research: the Women's Health Initiative (WHI). When its first findings were published in the early 2000s, they sent shockwaves through the medical community and caused a massive drop in HRT prescriptions.
The WHI was a huge, long-term study looking into the health effects of hormone therapy after menopause. The headline-grabbing finding was that women taking a specific combination of hormones—conjugated equine estrogens (CEE) and a synthetic progestin called medroxyprogesterone acetate (MPA)—had a higher rate of certain serious side effects. These included breast cancer, strokes, and blood clots.
But the devil was in the details, and those details often got lost in the panic. The real takeaway wasn't that all HRT was dangerous, but that this specific type of HRT carried these risks.
The most important distinction from the WHI study was this: the type of hormone matters. The increased risks were primarily tied to the combination of estrogen with a synthetic progestin (MPA). The risk profile for women taking estrogen alone was significantly different.
This discovery was a turning point. It forced medicine to shift away from a one-size-fits-all prescription and toward a much more personalized strategy.
Differentiating the Risks: Estrogen vs. Combination Therapy
The WHI study had two main groups, and the different results between them are the key to understanding HRT risks today.
- Estrogen-Plus-Progestin Therapy: This arm was for women who still had their uterus. They received both estrogen and the synthetic progestin (MPA). This is the group that showed a small but statistically significant increase in the risk of breast cancer, heart disease, stroke, and blood clots.
- Estrogen-Only Therapy: This group was for women who had a hysterectomy and didn't need progestin to protect their uterine lining. Their results were surprising. They showed no increased risk of heart disease and, even more unexpectedly, a lower risk of breast cancer than the women taking a placebo. The risk of stroke, however, was still slightly elevated.
This distinction is the cornerstone of how we manage HRT now. It became clear that the synthetic progestin used in the study was a major player in the negative outcomes. Since then, research has explored other options, like micronized progesterone, which is chemically identical to the progesterone our bodies make and appears to have a much better safety profile. Our comprehensive guide to hormone therapy for women dives deeper into how these treatment plans are now customized based on your unique health needs.
Today’s approach is far more nuanced. Doctors now carefully weigh your personal health history, your age, and whether you have a uterus to find the safest and most effective formula just for you.
A Realistic Look at HRT and Cancer Risk
Let's be honest: the word "cancer" in any medical conversation is enough to make anyone nervous. When it comes to Hormone Replacement Therapy (HRT), the supposed link to cancer has created so much confusion and fear that many women feel completely lost. It's time to cut through the noise, look at what the actual data says, and put those abstract percentages into a real-world context.
Getting clear on this isn't about causing anxiety. It's about giving you the clarity to weigh the incredible benefits of symptom relief against the potential downsides. The risk isn't some universal, one-size-fits-all number—it shifts depending on the type of hormones you take, how long you take them, and your own personal health story.
Breast Cancer Risk in Perspective
The most talked-about concern is, without a doubt, breast cancer. So, what does a "small increased risk" actually mean for you? Let's break down the numbers to make them tangible.
A major meta-analysis31709-X/fulltext) found a slight increase in breast cancer risk for each year a woman used HRT. To put this into perspective, for women who started HRT at age 50, the data suggests that after 5 years of use, there would be roughly 2 extra cases of breast cancer for every 1,000 women. This figure goes up to about 6 extra cases per 1,000 after 10 years and 12 per 1,000 after 15 years.
It's essential to remember that this risk isn't permanent. The data clearly shows that the elevated risk starts to fall as soon as you stop taking HRT, eventually returning closer to the baseline level of women who never used it.
For the vast majority of women on HRT for a few years, this means their personal increase in risk is very small. It’s a factor to consider, but it’s just one piece of a much larger health puzzle.
Protecting the Uterus: Endometrial Cancer
The connection between HRT and endometrial (uterine) cancer is a perfect example of why personalized treatment is so critical.
When estrogen is taken all by itself (unopposed estrogen), it stimulates the growth of the endometrium, which is the lining of the uterus. Over time, this constant stimulation can lead to abnormal cell growth and a significantly higher risk of endometrial cancer.
This is precisely why progestin is such a crucial part of HRT for any woman who still has her uterus.
- How Progestin Helps: Progestin acts as a counterbalance to estrogen. It signals the uterine lining to shed, much like a natural menstrual cycle.
- The Protective Effect: By preventing the endometrium from building up continuously, adding a progestin to estrogen therapy effectively cancels out the increased risk of uterine cancer, bringing it right back down to the level of women who don't use HRT.
This is a clear-cut case where the specific formula of your HRT is designed to manage a known risk. If you've had a hysterectomy, this risk doesn't apply to you, which is why estrogen-only therapy is often prescribed.
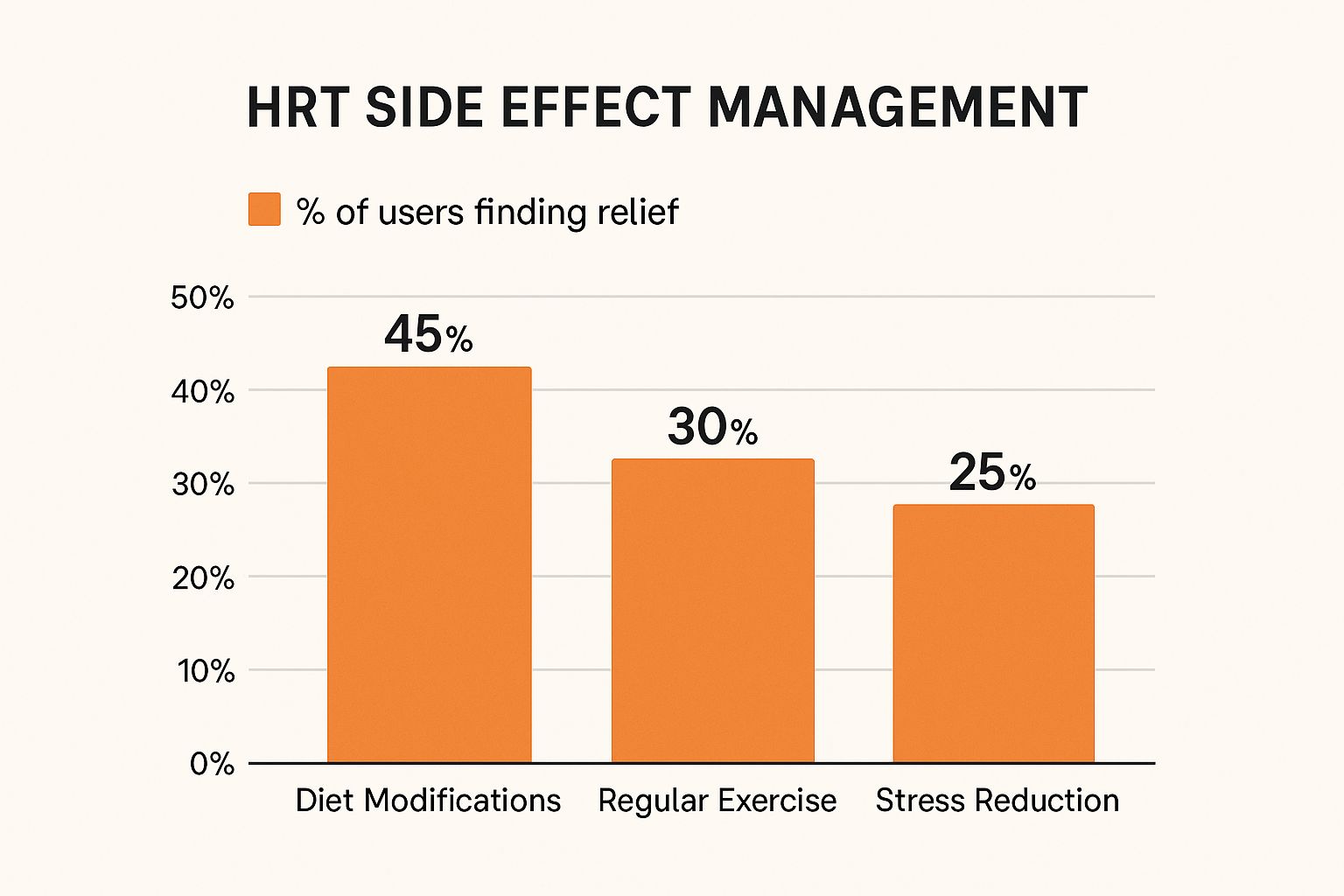
As this image shows, smart lifestyle adjustments can work hand-in-hand with medical strategies to manage side effects. Simple diet changes, for instance, are often a surprisingly effective tool for feeling better.
The Nuance of Ovarian Cancer Risk
The link between HRT and ovarian cancer is more subtle, but it's still an important part of the conversation.
Research suggests a small increase in risk, especially with long-term use of estrogen-only therapy. But the numbers here are quite small—translating to about one extra case of ovarian cancer for every 1,000 women who use HRT for five years.
Just like with breast cancer, this risk seems to fade after you stop therapy. This kind of information is a key part of the ongoing dialogue you should have with your doctor. Together, you can decide if the profound benefits HRT brings to your quality of life are a worthwhile trade-off for these small, but real, statistical risks.
To help you see the full picture at a glance, here’s a summary of how different HRT types relate to these cancer risks.
HRT and Cancer Risk Profile Summary
This table offers a comparative look at the risk levels associated with different types of cancer based on HRT formulation and usage.
| Cancer Type | Associated HRT Type | Risk Level Summary | Key Factor |
|---|---|---|---|
| Breast Cancer | Combined (Estrogen + Progestin), Estrogen-only | Slightly Increased. Risk rises with duration of use but decreases after stopping. The absolute increase is small for most users. | Duration of use. |
| Endometrial Cancer | Estrogen-only (unopposed) | Significantly Increased. Unopposed estrogen stimulates uterine lining growth, raising risk substantially. | Presence of progestin. |
| Endometrial Cancer | Combined (Estrogen + Progestin) | No Increased Risk. Progestin protects the uterine lining, neutralizing the risk from estrogen. | Balanced formulation. |
| Ovarian Cancer | Estrogen-only (long-term) | Slightly Increased. A very small increase in risk is noted, particularly with long-term estrogen-only therapy. | Duration and type of HRT. |
As you can see, the formulation of your HRT is the most critical factor in managing these risks. The "dangers" often highlighted in headlines are typically associated with specific situations, like taking unopposed estrogen when you still have a uterus—a practice that modern HRT protocols are explicitly designed to avoid.
Ultimately, understanding these nuances is what transforms fear into informed decision-making, allowing you and your provider to create a plan that is both safe and effective for you.
How to Minimize and Manage HRT Side Effects

Knowing the risks of hormone replacement therapy is only half the story. The other, far more empowering half is about actively working with your doctor to build a treatment plan that dials down those risks while turning up the benefits. This isn't something you just sit back and receive; it’s a partnership where your unique health profile and feedback are the most important guides.
Think of it as assembling a personalized toolkit to manage hormone replacement therapy side effects. The real goal isn't just to chase away symptoms. It's to find the safest, most effective strategy designed specifically for you. By taking a proactive role, you can have a massive impact on your treatment experience and your health for years to come.
The "Start Low, Go Slow" Principle
One of the golden rules in modern hormone therapy is to “start low and go slow.” The philosophy is as simple as it is effective: begin with the lowest dose possible that still brings you relief, and only increase it if you absolutely need to.
It’s like finding the perfect volume on your stereo. You don’t need to blast the music to hear it clearly; you just need it loud enough for you. Starting with a minimal dose gives your body a chance to ease into the change, which can head off many of those early adjustment side effects like headaches or bloating before they even start. This approach also ensures you're using the smallest amount of medication needed for the shortest time necessary—a cornerstone of managing long-term risks.
Your body is one of a kind, and your ideal dose will be, too. A dose that’s perfect for your friend might be way too high or too low for you. Regular check-ins with your doctor are for fine-tuning, keeping your prescription perfectly calibrated as your needs change.
How Delivery Method Changes Your Risk Profile
Not all HRT is created equal, and it turns out that how the hormones get into your body matters—a lot. The delivery method you and your doctor choose can fundamentally change your side effect profile, especially when it comes to serious risks like blood clots.
Oral HRT (Pills): When you swallow an estrogen pill, it has to pass through your liver first. This "first-pass metabolism" can trigger the liver to produce more clotting factors, which is why oral estrogen carries a slightly higher risk of blood clots (venous thromboembolism).
Transdermal HRT (Patches, Gels, Sprays): These methods are a game-changer. They deliver estrogen directly into your bloodstream right through the skin. By completely bypassing the liver, transdermal HRT does not appear to raise the risk of blood clots. For many women, particularly those with other risk factors for clots, this makes transdermal therapy a much safer first choice.
This single difference shows just how critical a personalized conversation is. Moving from a pill to a patch isn’t just about convenience; it’s a strategic medical choice that can directly lower your risk of a serious side effect.
Why the Type of Progestin Matters
For anyone with a uterus, taking a progestin is a non-negotiable part of combination HRT to protect the uterine lining. But just like with delivery methods, the specific type of progestin you use can make a real difference, especially when it comes to breast cancer risk and mood-related side effects.
The well-known WHI study, which raised many initial concerns, used a synthetic progestin called medroxyprogesterone acetate (MPA). Today, however, many experts prefer using micronized progesterone. This form is bioidentical, meaning it’s structurally the exact same as the progesterone your own body makes. While no hormone therapy is without risk, some studies suggest that micronized progesterone may have a better safety profile, particularly for breast health, compared to certain synthetic versions.
While progestin’s protective role for the uterus is well-established, it’s also important to have a clear view of all potential risks. For example, a major meta-analysis of over 50 studies found that postmenopausal estrogen therapy is linked to a small but real increase in the risk of ovarian cancer. The data showed that for every 1,000 women who begin estrogen therapy at age 50 and use it for five years, about one extra case of ovarian cancer would occur. You can read more about these findings and cancer risk to get the full picture.
By having these detailed conversations about dosage, delivery, and hormone type, you shift from being a passenger to being the co-pilot of your own HRT journey.
Frequently Asked Questions About HRT Side Effects
It’s completely normal to have questions when you’re thinking about Hormone Replacement Therapy (HRT). Even after you’ve gone over the common adjustments and bigger risks, some specific worries might linger. This section is here to give you straightforward, honest answers to the questions we hear most often about hormone replacement therapy side effects, so you can feel more confident and in control.
We'll tackle those nagging concerns head-on, from how long the initial side effects might stick around to the truth about weight gain and when to think about stopping treatment. Think of this as your go-to guide for those "what if" moments.
How Long Do HRT Side Effects Last?
One of the first questions on everyone's mind is, "Will these initial discomforts last forever?" The good news is that for the vast majority of women, the answer is a resounding no.
Most of the early side effects—things like breast tenderness, bloating, a bit of nausea, or headaches—are just temporary. They're part of your body's initial "getting to know you" phase with the new hormones and usually fade away within the first one to three months. Your system is simply recalibrating to a new normal.
If those feelings hang around for longer or feel particularly intense, it's time for a chat with your doctor. Often, a simple tweak is all that's needed. Your doctor might suggest:
- Adjusting your hormone dosage
- Changing the time of day you take your HRT
- Switching from a pill to a patch or gel to see if that helps
It's also important to separate these temporary adjustments from the much rarer, more serious health risks like blood clots. Those risks don't just disappear over time. Instead, they’re managed from day one by sticking to the core principle of modern HRT: using the lowest effective dose for the shortest necessary time and having regular check-ins with your doctor to make sure the benefits continue to outweigh any risks.
Can Hormone Replacement Therapy Cause Weight Gain?
The fear of gaining weight is a huge concern for many women considering HRT, but the link isn't as direct as you might think. While it’s true that many women notice weight changes during menopause, HRT is almost never the main culprit.
Research consistently shows that HRT itself doesn’t directly cause any significant, long-term weight gain. What's really going on is more tied to the natural process of aging. Things like a slowing metabolism, a natural decline in muscle mass, and shifts in how the body stores fat are the real drivers behind the changing number on the scale during this life stage.
Some women do notice temporary fluid retention or bloating when they first start HRT, especially with oral estrogen. This can make the scale tick up a few pounds, but it's usually just water weight that resolves as your body adjusts.
In fact, HRT can actually be an ally in your weight management efforts. By tackling disruptive menopause symptoms like poor sleep, low energy, and mood swings, it can give you the boost you need to stay active and make healthy food choices—which are the true keys to managing your weight during menopause and beyond.
Are Bioidentical Hormones a Safer Option?
The term "bioidentical" is a huge buzzword in HRT conversations, often marketed as a more "natural" and therefore "safer" choice. While it sounds great on the surface, it's important to know what that word really means—and what it doesn't.
"Bioidentical" simply means the hormones in a product, like estradiol or micronized progesterone, are chemically identical to the ones your body produces. The thing is, many standard, FDA-approved HRT products already use these bioidentical hormones. The real controversy usually centers on custom-compounded bioidentical hormones. These are special formulations mixed at compounding pharmacies based on a doctor's specific prescription, often after saliva testing. They are not regulated by the FDA with the same rigorous standards as mass-produced medications.
As of now, there is no large-scale, credible scientific evidence showing that these custom-compounded formulas are any safer or have fewer side effects than standard, FDA-approved HRT. Any form of hormone therapy, no matter where it comes from, carries similar potential risks and needs careful medical supervision. Your safety ultimately hinges on getting the right, scientifically tested dose and formulation for your body—not on a "bioidentical" label alone.
When Is the Right Time to Stop Taking HRT?
There’s no magic expiration date for HRT. Deciding when to stop is a deeply personal choice, one you should make in close partnership with your doctor.
The guiding principle is to re-evaluate your treatment every year. Together, you and your doctor will weigh the benefits you're still getting against any potential long-term risks. For some women, a few years on HRT is enough to get them through the worst of their menopause symptoms, and they might choose to slowly taper off their dose.
For other women, especially those dealing with persistent, severe symptoms like disruptive hot flashes or a high risk of osteoporosis, staying on HRT longer might be the best path forward for their quality of life. The decision always comes down to your individual health, the severity of your symptoms, and how you feel. It's an ongoing conversation, not a final destination.
Navigating the world of hormone therapy can feel complex, especially when it comes to acquiring treatment safely and legally. For those looking to understand the process better, our guide on how to buy hormone and testosterone therapy online offers a clear roadmap.
At Elite Bioscience, we are dedicated to providing clear, medically sound information and therapies to help you make empowered decisions about your health. If you are ready to explore personalized treatment options designed for your unique needs, we invite you to take the next step.