The shift into postmenopause isn't a single event, but a profound hormonal transition. It brings a wide range of changes, from the infamous hot flashes and mood swings to more subtle issues like vaginal dryness and restless nights. These aren't random occurrences; they're all connected to the sharp decline of estrogen.
Decoding the Postmenopause Experience
After your final period, your body's hormonal landscape is permanently altered. For decades, estrogen acted as a master conductor, leading a complex orchestra of bodily functions. It managed everything from your body temperature and mood to your bone density and skin health.
When this conductor steps down, the orchestra can fall out of sync. This is why women experience such a wide array of symptoms—from physical to emotional—all at once. This hormonal shift is a completely natural biological process, not a sign of illness. But its effects can feel deeply disruptive. Understanding that these symptoms are rooted in a specific physiological change is the first real step toward managing them.
Why Do Symptoms Vary So Much?
One of the biggest questions we hear is, "Why are my symptoms so intense when my friend barely noticed a thing?" The answer is that estrogen's influence is incredibly far-reaching. Its receptors are found in almost every system of the body:
- In the brain: Where it helps regulate mood, memory, and your internal thermostat.
- In the skin: Where it supports collagen production to maintain elasticity.
- In the bones: Where it plays a critical role in maintaining strength and density.
- In the urogenital tract: Where it keeps tissues moist, elastic, and healthy.
Because its reach is so extensive, a drop in estrogen can trigger a cascade of seemingly unrelated issues. It’s the reason you might be dealing with achy joints, brain fog, and hot flashes all at the same time. For a clear, personalized picture of your hormonal profile, advanced diagnostics like the DUTCH hormone test can provide detailed insights.
The Most Common Signal Your Body Sends
Of all the signs of low estrogen, the most notorious are vasomotor symptoms—better known as hot flashes and night sweats. These are often the first and most prominent indicators that your estrogen levels are dropping.
Globally, an estimated 40% to 80% of postmenopausal women report dealing with hot flashes, which feel like a sudden, intense wave of heat spreading through the body. Their frequency and severity are usually at their peak in the first few years after menopause. You can read the full research about vasomotor symptoms to learn more.
These symptoms are more than just an inconvenience. They are your body's direct response to the brain's struggle to regulate temperature without its hormonal guide. Recognizing them as a biological signal can help demystify the experience and empower you to seek the right solutions.
Common Low Estrogen Symptoms at a Glance
Navigating the symptoms of low estrogen can feel overwhelming because they affect so many different parts of the body. The table below provides a quick summary to help you connect the dots between what you're feeling and the body system being affected.
| Symptom Category | Common Examples | Primary Body System Affected |
|---|---|---|
| Vasomotor | Hot flashes, night sweats, sudden chills | Central Nervous System |
| Urogenital | Vaginal dryness, painful intercourse, urinary urgency | Genitourinary System |
| Psychological | Mood swings, anxiety, irritability, brain fog | Neurological & Endocrine System |
| Musculoskeletal | Joint pain, loss of bone density, muscle aches | Skeletal & Muscular Systems |
| Dermatological | Dry skin, thinning hair, brittle nails | Integumentary System |
This is just a snapshot, but it illustrates how a single hormonal change can have such a wide-ranging impact. Understanding these connections is the first step toward finding targeted, effective relief.
Recognizing the Most Common Physical Symptoms
After menopause, the physical signs of low estrogen are often the most obvious and disruptive. It’s easy to feel like you’re dealing with a dozen disconnected problems, but many of them trace back to the same root cause: a major drop in your body's primary female hormone.
Getting a handle on these tangible changes is the first step toward understanding what’s happening in your body and finding the right way forward.

The classic symptoms everyone talks about are hot flashes and night sweats, known together as vasomotor symptoms. Imagine you’re trying to sleep or giving a presentation, and out of nowhere, an intense wave of heat floods your chest, neck, and face. This isn't just feeling a bit warm; it’s a powerful, full-body furnace blast that can leave you drenched in sweat, flushed, and completely flustered.
Night sweats are just hot flashes that crash the party while you're sleeping. They can be so intense that they soak your pajamas and sheets, forcing you to wake up and change. It’s no wonder sleep quality takes a nosedive for so many women after menopause.
Understanding Genitourinary Syndrome of Menopause
Beyond the internal thermostat going haywire, low estrogen dramatically affects the tissues in your urinary and genital areas. This collection of symptoms has a clinical name: Genitourinary Syndrome of Menopause (GSM).
Estrogen is the hormone that keeps the vaginal and urinary tissues healthy, elastic, and lubricated. When it disappears, these tissues can become thinner, drier, and much more fragile.
This isn't just a minor annoyance; it's a progressive condition that can impact your comfort, intimacy, and urinary health. GSM symptoms are incredibly common, but they're often the last thing anyone wants to talk about.
The key signs of GSM include:
- Vaginal Dryness and Itching: A persistent feeling of soreness, burning, or general discomfort in the vaginal area.
- Painful Intercourse (Dyspareunia): Without natural lubrication and with thinning tissues, sexual activity can become uncomfortable or even painful.
- Urinary Urgency and Frequency: A sudden, powerful need to urinate more often, even when your bladder isn't actually full.
- Recurrent Urinary Tract Infections (UTIs): Changes in the urinary tract’s lining make it more vulnerable to bacterial infections.
Even though it’s widespread, GSM is often missed by doctors. Research shows that while up to 70% of women may have GSM symptoms, less than 10% ever bring it up with their doctor, usually because of embarrassment or the mistaken belief that it’s just an inevitable part of getting older. You can discover more insights about this common condition and why it's so undertreated.
Changes to Your Skin, Hair, and Joints
The effects of low estrogen ripple out to your body's structural components, too, changing everything from how your skin looks to how your joints feel.
Think of estrogen as a key supporter of collagen—the protein that gives your skin its bounce and firmness. When estrogen levels plummet, so does collagen production. This causes noticeable changes that many women chalk up to aging alone, but hormones are a huge part of the story.
You might notice your skin becoming:
- Drier and Thinner: It can feel less supple and become more prone to fine lines and wrinkles.
- More Prone to Bruising: Thinner skin offers less padding for the delicate blood vessels just beneath the surface.
Your hair doesn't get a pass, either. Estrogen helps keep hair in its growing phase for a longer period. With less of it around, hair follicles can shrink, leading to slower growth and more shedding. For many, this results in noticeably thinning hair, especially on the scalp.
The Connection to Aches and Pains
If you’ve noticed more nagging joint pain or stiffness since hitting menopause, you are definitely not alone. Estrogen has natural anti-inflammatory properties and helps maintain the health of cartilage, the soft cushion between your joints.
As estrogen levels decline, inflammation can creep up while joint lubrication goes down. This often translates to aches and pains in the knees, hips, shoulders, and hands. Many women describe it as a dull, persistent ache that’s worse first thing in the morning or after sitting for a while.
Recognizing these diverse physical symptoms—from hot flashes and urinary issues to thinning hair and achy joints—as interconnected signs of low estrogen is the first step. It validates that what you're feeling is real, it’s hormonally driven, and most importantly, it's something you can manage with the right approach.
How Low Estrogen Impacts Your Mood and Mind
We talk a lot about the physical side of low estrogen after menopause—the hot flashes, the sleep issues. But the impact on your mental and emotional well-being can be just as profound, and frankly, sometimes more disorienting.
If you’ve been feeling irritable, anxious, or like your brain is wrapped in a thick fog, you are absolutely not alone. These shifts aren’t a personal failing or a sign you're "losing it." They are a direct, biological result of the hormonal changes happening inside your brain.
Think of estrogen as a master conductor for your brain's orchestra of neurotransmitters. It works closely with chemical messengers like serotonin (the mood stabilizer) and dopamine (the motivation molecule) to keep everything in harmony. When estrogen levels drop, it’s like the conductor suddenly walked off stage, leaving these crucial chemicals out of sync.
This disruption can unleash a cascade of emotional and cognitive challenges that can feel bewildering and intensely frustrating.

Navigating Mood Swings and Increased Anxiety
One of the most common psychological symptoms women report is a sharp increase in emotional volatility. You might find yourself snapping at a loved one over something trivial or being blindsided by a wave of sadness that seems to come from nowhere. This isn’t a change in your personality; it's a change in your brain chemistry.
Without estrogen's steadying hand, the systems that regulate your emotional responses can become much more sensitive. This can show up in a few key ways:
- Irritability and Anger: Small frustrations that you used to brush off can suddenly feel monumental, triggering an outsized, flash-of-anger response.
- Anxiety and Panic: Many women describe a new or worsening sense of general anxiety—that constant, humming worry—or even experience full-blown panic attacks for the first time.
- Feelings of Sadness: A persistent low mood or feeling like you're perpetually on the verge of tears can become a frequent, unwelcome companion.
These feelings are often amplified by other menopausal symptoms, like poor sleep and hot flashes. It creates a vicious cycle where physical discomfort fuels emotional distress, which in turn makes it even harder to cope with the physical symptoms.
This connection is well-documented. Research shows women in the menopausal transition are 2.5 times more likely to experience a major depressive disorder. You can learn more about the link between menopause and mood disorders from in-depth clinical studies on the topic.
Clearing the Confusion of Brain Fog
Beyond your mood, one of the most maddening mental symptoms is "brain fog." While it's not an official medical term, it perfectly captures the feeling of being mentally sluggish, forgetful, and unable to concentrate.
You might walk into a room and completely forget why you’re there, struggle to find the right word in a conversation, or find it nearly impossible to focus on a task you used to handle with ease.
Brain fog is not a sign of permanent cognitive decline. It's a temporary disruption caused by hormonal shifts. Estrogen plays a vital role in crucial brain functions like memory recall, executive function, and verbal fluency.
These cognitive complaints are incredibly common. Some studies indicate that up to 60% of women report difficulties with memory and concentration during this time. The dip in estrogen affects the efficiency of your neural pathways, essentially slowing down your brain's processing speed.
This can be especially distressing at work or in social situations, often leading to a painful loss of confidence. But recognizing brain fog as a real, physiological symptom of low estrogen is the first step toward managing it with patience and self-compassion. The key takeaway here is that these mental and emotional hurdles are a shared experience, rooted firmly in biology—not in your capabilities.
The Toll on Sleep Quality and Energy Levels
Beyond the hot flashes and mood swings, there's a silent struggle that often defines the postmenopausal experience: profound exhaustion. For many women, poor sleep and persistent fatigue aren't just minor annoyances; they become a relentless cycle that drains the joy and vitality from daily life.
This deep-seated fatigue is directly wired to the hormonal shifts that throw your body's natural sleep-wake cycles into chaos. Think of estrogen as a key player in promoting calm, restorative rest. When its levels drop, your sleep architecture can become unstable, making it much harder to get the deep, uninterrupted sleep your body and brain are desperate for.

The Direct Link Between Night Sweats and Broken Sleep
The most infamous culprit behind postmenopausal sleep problems is, of course, night sweats. Waking up suddenly, drenched and overheated, is more than just uncomfortable—it's a violent interruption that shatters your sleep cycle. Each time it happens, you're yanked out of deep or REM sleep, forcing your brain to start the whole process over again.
Just a few of these episodes a night are enough to rack up a massive "sleep debt." You end up waking in the morning feeling like you haven't slept at all, no matter how many hours you actually spent in bed.
When Sleep Suffers Even Without Sweats
But night sweats are only half the story. The loss of estrogen itself can directly mess with your brain's sleep-regulating centers, even on nights when you're not having hot flashes. This hormonal void can create a state of hyperarousal, making it incredibly difficult to fall asleep in the first place or causing you to wake up frequently for no apparent reason.
It's no surprise that sleep disturbances are a top complaint, affecting an estimated 40-60% of postmenopausal women. While night sweats are a huge factor, the estrogen drop alone can disrupt the sleep cycle. Many women find it takes longer to fall asleep and they get less REM sleep, which leads to non-restorative rest and crushing daytime fatigue. To dive deeper, you can learn more about menopause and sleep from the Sleep Foundation.
It's a cruel paradox: you're bone-tired, but you just can't get the quality sleep you need to recharge. This isn't a personal failure; it's a physiological response to a fundamental hormonal shift.
The Domino Effect on Daily Life
This chronic lack of quality sleep creates a powerful domino effect that touches every part of your day. The fatigue it causes isn't just "feeling tired"—it's a profound lack of energy that can make even the simplest tasks feel like climbing a mountain.
This exhaustion then acts as an amplifier for other symptoms of low estrogen postmenopausal, including:
- Worsened Brain Fog: A sleep-deprived brain struggles with cognitive function, making memory lapses and concentration issues feel even more severe.
- Increased Moodiness: Poor sleep shortens your emotional fuse, leaving you more vulnerable to irritability, anxiety, and feeling completely overwhelmed.
- Reduced Physical Stamina: Without proper rest, your body can't repair itself, which can lead to more muscle aches and a general sense of physical weakness.
In the end, poor sleep and the fatigue that follows aren't just isolated issues. They are central to the postmenopausal experience, making every other symptom feel that much harder to handle. Recognizing this connection is the first critical step toward reclaiming your energy and feeling like yourself again.
The Long-Term, Silent Risks of Low Estrogen
The immediate symptoms of menopause, like hot flashes and night sweats, are impossible to ignore. They’re loud, disruptive, and demand your attention right now. But once the dust settles, it’s just as crucial to turn your focus to the quiet, long-term health shifts that happen in the background.
Think of estrogen as a silent but powerful guardian for several of your body’s most critical systems. When its presence fades, those systems are left more vulnerable. This isn’t a reason to be alarmed—it's a reason to be proactive. Understanding these risks gives you the power to protect your health for decades, turning conversations with your doctor from reactive to preventative.
Your Bones: The Silent Remodeling Project
One of estrogen’s most important, behind-the-scenes jobs is managing your bone health. It’s like a master foreman on a construction site, perfectly balancing the demolition of old bone (resorption) with the building of new bone (formation). When estrogen leaves the job site, that delicate balance is shattered. The demolition crew starts working overtime, breaking down bone far faster than it can be rebuilt.
This imbalance leads to a gradual, invisible loss of bone density. Your bones become more porous and fragile, a condition called osteoporosis. The decade after menopause is a particularly critical window. In fact, women can lose up to 20% of their bone density in just the first 5-7 years after menopause, which dramatically increases the risk of fractures. You can find more details about this condition at the Bone Health and Osteoporosis Foundation.
This is why postmenopausal women are so much more susceptible to fractures from a minor fall or even a simple bump, especially in the hip, spine, and wrist.
Osteoporosis is often called a "silent disease" for a good reason—it progresses without any obvious symptoms until a bone breaks. This makes proactive screening and regular discussions with your doctor absolutely essential for your long-term well-being.
Your Heart: Losing a Key Protector
Estrogen also plays a vital protective role in your cardiovascular system. It helps keep your blood vessels flexible, which promotes healthy blood flow, and it’s a key player in managing your cholesterol levels—keeping the "bad" LDL cholesterol down while supporting the "good" HDL cholesterol.
Once that hormonal protection is gone, several changes can start to happen that impact your heart health:
- A Shift in Cholesterol: LDL cholesterol often begins to climb while HDL levels may drop, creating conditions that are more favorable for plaque to build up in your arteries.
- Stiffer Blood Vessels: Without estrogen's influence, blood vessels can become less elastic and may not dilate as easily, which can contribute to higher blood pressure.
- Changing Body Fat: Many women notice that weight starts to accumulate around the abdomen instead of the hips and thighs. This type of deep belly fat, known as visceral fat, is a well-known risk factor for heart disease.
Together, these changes significantly raise the risk for cardiovascular events like heart attacks and strokes. Understanding this connection is the first step toward taking control. By addressing the underlying hormonal shifts, you can make a huge impact on your long-term wellness strategy. You can learn more about the benefits of hormone replacement therapy in our detailed guide.
By staying on top of bone density screenings, getting regular heart health check-ups, and talking with your doctor about preventative care, you can actively manage these long-term risks. Recognizing that these potential health issues are also symptoms of postmenopausal low estrogen is empowering—it allows you to take charge of your future health.
Finding Relief and Creating a Treatment Plan
Navigating the sheer number of symptoms that come with low estrogen can feel completely overwhelming, but I want to be clear: relief is absolutely possible. You don't have to just grit your teeth and endure the discomfort.
The first step is always the most important—partnering with a healthcare provider to map out a strategy that actually fits your health, your lifestyle, and what you want for your future.
So, when is it time to make that call? If your symptoms are getting in the way of your life—whether it's night sweats that ruin your sleep, painful intimacy, persistent brain fog, or mood swings that feel out of control—it's time to talk to a professional. A proper evaluation will confirm that low estrogen is the real culprit and rule out anything else that might be going on.
Preparing For Your Doctor's Visit
To get the most out of your appointment, you need to come prepared. This isn't just about rattling off a list of complaints; it's about painting a clear, detailed picture of what you're experiencing.
Before you go, try tracking these things:
- Symptom Log: Make a note of what symptoms you're having, how often they pop up, and how bad they are on a scale of 1 to 10.
- Triggers: Start to notice what makes things worse. Does caffeine or a glass of wine set off a hot flash? Does stress make your anxiety spike?
- Your Goals: What do you truly want to get back? Is it a full night of uninterrupted sleep? Less anxiety? A more comfortable sex life? Being crystal clear on your priorities helps your doctor focus on what matters most to you.
This simple preparation turns your visit from a standard check-up into a true strategy session. It empowers you to work side-by-side with your doctor to find solutions that will make a real difference.
An Overview of Treatment Approaches
Once you've decided to seek help, you'll discover there are several proven paths to managing the symptoms of low estrogen after menopause. The right approach for you will likely be a mix of strategies, tailored to your specific situation.
The main treatment categories are lifestyle adjustments, Hormone Therapy (HT), and non-hormonal medications. Think of lifestyle changes—like tweaking your diet and getting more exercise—as the foundation of any plan. They can be surprisingly effective for milder symptoms and are fantastic for your overall health.
For more moderate to severe symptoms, medical treatments are often the game-changer. Hormone Therapy is widely considered the gold standard for tackling things like hot flashes and night sweats, and it also offers powerful protection against osteoporosis. It works by simply giving your body back the estrogen it's missing. You can explore the different estrogen replacement therapy options in our detailed guide to get a better sense of how they work.
For women who either can't or prefer not to use hormones, there are also excellent non-hormonal medications that can bring significant relief, especially for those disruptive vasomotor symptoms.
The table below breaks down these different avenues, giving you a clearer picture of how each one works.
Comparing Treatment Approaches for Low Estrogen Symptoms
This table provides a comparative overview of common treatment strategies, their primary targets, and key considerations to help you understand the landscape of available options.
| Treatment Approach | Primary Symptoms Targeted | Key Considerations |
|---|---|---|
| Lifestyle Adjustments | Mild hot flashes, mood swings, sleep disturbances. | Safest option with broad health benefits. Effects are gradual and may not be sufficient for severe symptoms. |
| Hormone Therapy (HT) | Moderate to severe hot flashes, night sweats, vaginal dryness, bone loss. | Most effective treatment for vasomotor symptoms. Requires a thorough medical evaluation to assess risks and benefits. |
| Non-Hormonal Medications | Moderate to severe hot flashes and night sweats. | Good alternative for women who cannot or choose not to use hormones. May have different side effect profiles. |
Ultimately, the goal is to find the right combination that aligns with your body and your personal preferences.
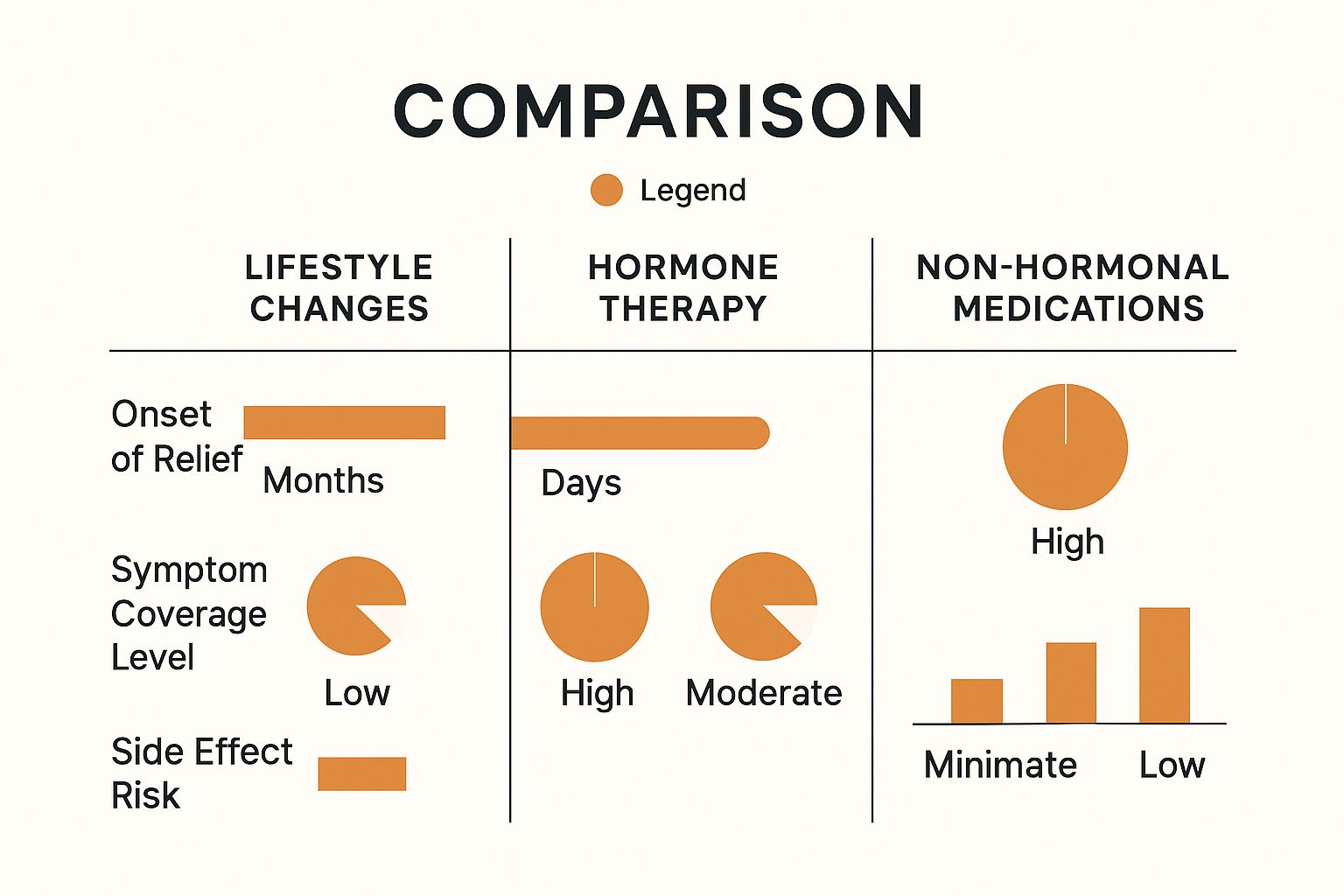
As you can see, there's a bit of a trade-off. Hormone therapy tends to offer the quickest and most comprehensive relief but comes with risks that need to be discussed. Lifestyle changes are the safest path but are slower and might not be powerful enough on their own. The best way forward is always a personalized one, created with a knowledgeable provider who sees your whole health picture.
Your Postmenopause Questions, Answered
Once you've officially crossed the finish line of menopause, it's completely normal to still have questions. Let's clear up some of the most common uncertainties about what comes next, from how long symptoms might stick around to what your treatment options really are.
How Long Do Symptoms Last After Menopause?
This is the million-dollar question, and the answer is different for everyone. Hot flashes and night sweats—the classic vasomotor symptoms—are usually at their worst in the first few years, but they can hang around for an average of 7-10 years. For some women, they may even last longer.
It's a common myth that all symptoms just fade away. Other issues, especially those tied to genitourinary health (like vaginal dryness) and bone density loss, are progressive. Without proactive management, these symptoms can continue and even worsen over time.
Are My Symptoms From Perimenopause or Postmenopause?
The real difference-maker here is your menstrual cycle. Perimenopause is the transition—the runway leading up to your final period. Your hormones are all over the place during this time, causing irregular cycles right alongside those classic low-estrogen symptoms.
Postmenopause, on the other hand, officially kicks in exactly 12 consecutive months after your last period. The symptoms can feel very similar, but the key distinction is hormonal: in postmenopause, your estrogen levels are consistently low, not wildly fluctuating like they were before.
Is Hormone Therapy My Only Option for Severe Symptoms?
Absolutely not. While Hormone Therapy (HT) is often called the gold standard for treating moderate to severe symptoms like hot flashes and preventing osteoporosis, it is far from your only choice.
For women who can't take hormones, or simply prefer not to, there are several excellent alternatives:
- Non-Hormonal Medications: There are FDA-approved prescription drugs specifically designed to effectively manage hot flashes and night sweats.
- Localized Estrogen: For symptoms centered around vaginal dryness and urinary issues, localized therapies are a game-changer. These creams, rings, or tablets deliver a low dose of estrogen directly to the tissues that need it, with minimal absorption into the rest of your body.
Every woman's journey is unique, and your treatment plan should be, too.
At Elite Bioscience, we provide advanced therapies to help you manage your health with confidence. Our telehealth platform offers convenient access to personalized treatments designed to restore your vitality and well-being. Discover how our tailored solutions can support you by visiting us online today.