The real difference between HRT and TRT boils down to scope. Think of it like this: Hormone Replacement Therapy (HRT) is a broad-spectrum approach, like a general contractor managing a whole-house renovation. In contrast, Testosterone Replacement Therapy (TRT) is a specialist, like an electrician brought in for one specific job—restoring testosterone.
HRT vs TRT Unpacking The Core Differences
It's a common mistake to think of HRT and TRT as interchangeable terms, but they really aren't. They serve different patient populations, target different hormones, and have entirely different goals. One aims for a comprehensive hormonal balance, while the other is all about targeted restoration of a single, powerful hormone.
A Closer Look at Each Therapy
When most people hear HRT, they immediately think of women going through menopause. In that classic context, the therapy focuses on supplementing estrogen and progesterone to manage symptoms like hot flashes, mood swings, and poor sleep.
However, HRT isn't just for women. Some men undergo a broader form of hormone therapy—sometimes called "hormone optimization"—to address declines in multiple hormones, not just testosterone.
TRT, on the other hand, is laser-focused. It's a specific medical treatment prescribed almost exclusively for men who have been diagnosed with clinical hypogonadism, or low testosterone. Its sole purpose is to bring testosterone levels back into a healthy, functional range to combat symptoms like fatigue, low libido, and loss of muscle mass. The key distinction is in what hormones are being replaced and for whom. You can read more about the distinctions between HRT and TRT at hormonesandwellness.com.
To make this crystal clear, here’s a quick side-by-side breakdown.
Quick Comparison HRT vs TRT
This table provides a simple, at-a-glance summary of the primary distinctions between Hormone Replacement Therapy and Testosterone Replacement Therapy.
| Attribute | Hormone Replacement Therapy (HRT) | Testosterone Replacement Therapy (TRT) |
|---|---|---|
| Primary Goal | To restore balance across multiple hormones. | To specifically restore testosterone to optimal levels. |
| Target Hormones | Primarily estrogen & progesterone; may include testosterone, DHEA. | Exclusively testosterone. |
| Typical Patient | Women in perimenopause/menopause; men with multiple deficiencies. | Men diagnosed with clinical hypogonadism (low T). |
| Treatment Scope | Broad and comprehensive. | Highly specific and targeted. |
Getting this fundamental difference right is the first and most important step. It helps you understand which therapeutic path might actually be relevant to your unique health needs and long-term goals.
Understanding Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy, or HRT, is a medical treatment designed to replenish hormones that your body is no longer making in adequate amounts. While most people immediately think of women and menopause, HRT is actually a broad umbrella term for any protocol aimed at restoring hormonal balance to improve health and quality of life.

Its most well-known use is helping women navigate the disruptive symptoms of menopause. As the ovaries wind down their production of estrogen and progesterone, women can be hit with a wave of symptoms—hot flashes, night sweats, vaginal dryness, and mood swings—that can seriously degrade their well-being.
HRT works to counteract these issues by reintroducing those key hormones, offering significant relief. If you want to dive deeper into the basics, our guide on what is hormone replacement therapy is a great place to start.
Beyond Menopause Applications
While menopause is the number one reason women turn to HRT, its applications are much broader. The ultimate goal is always to bring the body's hormones back into a healthy equilibrium, which can benefit a wide range of people.
- Andropause in Men: Some men experience a dip in more than just testosterone. For them, a comprehensive HRT plan can address these wider deficiencies—sometimes called "male menopause"—for a more complete return to wellness.
- Gender-Affirming Care:HRT is a fundamental part of the medical transition for transgender individuals. It helps align their physical characteristics with their gender identity in what is a critical, life-affirming application of hormone therapy.
A Controversial History Reshaping Modern Practice
The public perception of HRT was turned upside down in 2002 by the Women’s Health Initiative (WHI) study, which seemed to link the therapy to increased health risks. After its release, HRT use plummeted by over 60% as a wave of fear washed over hormone supplementation. However, later analysis has suggested this massive drop in estrogen therapy might be connected to tens of thousands of excess deaths among women, underscoring the delicate balance between risk and reward. You can read the full research about these post-WHI findings.
This historical context is vital because it forced a major shift toward more personalized and cautious HRT protocols. Today's approach is a world away from the old one-size-fits-all model, focusing instead on highly individualized treatment plans.
Modern HRT isn't just about topping off one or two hormones. Clinicians now rely on detailed lab work and symptom analysis to craft balanced protocols tailored to the individual. A woman's HRT plan might restore estrogen and progesterone, but it could also include a small, strategic dose of testosterone to boost energy and libido. This nuanced approach highlights the clear difference between HRT and TRT; HRT is about orchestrating a hormonal symphony, not just turning up the volume on a single instrument.
Understanding Testosterone Replacement Therapy (TRT)
While Hormone Replacement Therapy (HRT) can feel like a broad hormonal balancing act, Testosterone Replacement Therapy (TRT) is a much more focused medical treatment. It has one clear objective: to bring testosterone levels back to a healthy range in men diagnosed with clinical hypogonadism, more commonly known as Low T. This isn’t a wellness trend; it’s a specific solution for a recognized medical condition.
Men dealing with low testosterone often face a frustrating cluster of symptoms that can quietly sabotage their daily lives. These issues are too often brushed off as just a normal part of getting older, but they frequently point to an underlying hormonal problem that can be fixed.
Recognizing The Signs Of Low Testosterone
The symptoms of hypogonadism can be both physical and mental, creating a ripple effect that impacts everything from your energy at the gym to your personal relationships.
Common signs include:
- Chronic Fatigue: A deep, persistent exhaustion that no amount of rest seems to fix.
- Low Libido: A noticeable drop in sex drive and overall sexual function.
- Reduced Muscle Mass: Finding it harder to build or even maintain muscle, despite working out.
- Mood Instability: An increase in irritability, brain fog, or even feelings of depression.
Because these symptoms tend to creep in gradually, it's easy to miss the real cause. But when Low T is properly diagnosed and treated, the turnaround can be life-changing. TRT has seen a massive surge in popularity for this very reason; in the United States alone, spending doubled from $1 billion to $2 billion between 2008 and 2012.
The effectiveness of this targeted therapy is a huge part of its story. Studies show that about 85% of men on TRT find it effective, with 75% reporting a better quality of life and 71% noticing improved mental wellbeing. You can discover more insights about these TRT outcomes and their impact.
Key Considerations and Long-Term Commitment
Despite its high success rate, TRT is not a quick fix. It’s a lifelong commitment. Once you start, your body’s own testosterone production often shuts down, which means you need to stay on therapy to keep your levels optimized and prevent symptoms from returning.
This long-term requirement is a primary reason why some men stop treatment. On top of that, historical safety concerns once prompted the FDA to issue guidance, highlighting just how important proper medical supervision is. Understanding the difference between HRT and TRT is crucial here; TRT’s focused nature means your doctor must diligently monitor specific health markers, like red blood cell counts and prostate health, to ensure the therapy is safe and effective for the long haul. A qualified physician will build a protocol that manages these variables right from the start.
Comparing HRT and TRT Protocols
While the core difference between HRT and TRT comes down to the hormones involved, how these therapies are applied in the real world reveals even bigger distinctions. The day-to-day experience, from who gets the treatment to how it's administered, is tailored to achieve very different goals.
Think of it this way: HRT is about restoring a delicate hormonal balance, usually by addressing multiple hormones at once. On the other hand, TRT has a laser focus on one thing: bringing testosterone levels back into a healthy, optimal range.
Patient Profiles and Primary Goals
The typical patient for each therapy really tells the story. HRT is most often prescribed for women navigating perimenopause or menopause. Their goal is broad relief from a whole host of symptoms—hot flashes, mood swings, brain fog, and poor sleep—by replenishing dwindling estrogen and, in many cases, progesterone.
In contrast, the usual TRT patient is a man diagnosed with clinical hypogonadism, or low testosterone. He’s looking to fix symptoms directly tied to that deficiency, like persistent fatigue, loss of muscle mass, zero libido, and mental fogginess. While both patients want to feel better, the hormonal paths they take are completely different.
The key takeaway is purpose-driven treatment. HRT orchestrates a hormonal symphony to address systemic issues, primarily in women. TRT is a precision tool used to fix a specific deficiency, almost always in men.
Administration Methods A Side-by-Side Look
The methods used to deliver these hormones are just as varied as their goals. The right choice often comes down to the specific hormone being used, patient preference, and the need for a steady, consistent release into the body. An effective treatment plan is only as good as its delivery method.
To help visualize these differences, the table below breaks down the common protocols for both HRT and TRT. It makes it clear why certain methods are favored for specific therapies and what patients can realistically expect.
HRT vs TRT Side-by-Side Protocol Comparison
| Aspect | Hormone Replacement Therapy (HRT) | Testosterone Replacement Therapy (TRT) |
|---|---|---|
| Common Methods | Pills, patches, gels, vaginal rings, pellets | Injections, gels, creams, patches, pellets |
| Method Rationale | Patches and gels offer steady estrogen absorption, while pills are common. Vaginal rings provide localized relief. | Injections are highly effective for stable levels. Gels are popular for daily application but risk transference. |
| Frequency | Daily (pills, gels), twice-weekly (patches), or every few months (pellets, rings). | Daily (gels), weekly/bi-weekly (injections), or every 3-6 months (pellets). |
As you can see, the daily management and long-term experience can differ quite a bit depending on the therapy and chosen delivery system.
This infographic gives a great snapshot of the kind of positive outcomes men often experience with a well-managed TRT protocol, showing just how effective it can be in key areas of life.
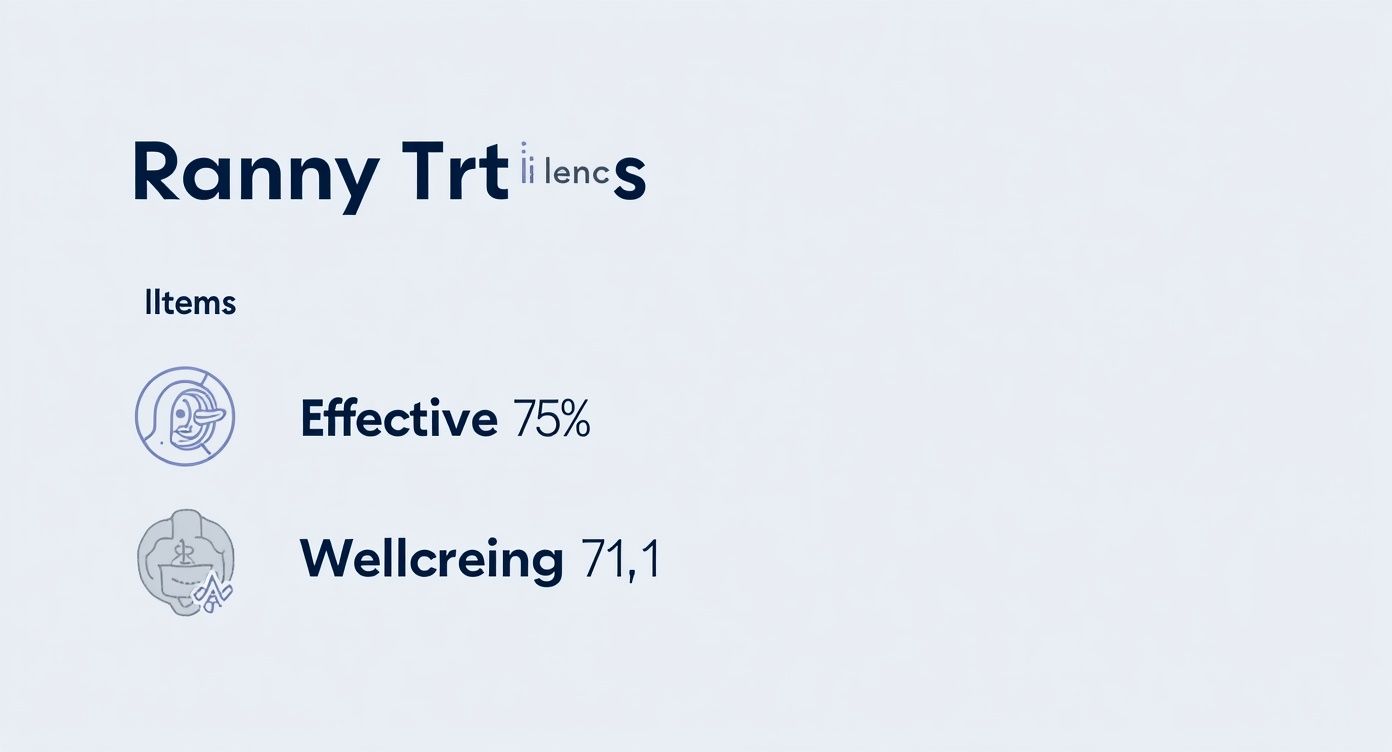
The data speaks for itself: with a 75% effectiveness rate and a well-being score of 71.1, the right TRT plan can deliver massive improvements to a man's quality of life. For anyone considering treatment, learning more about the various testosterone replacement therapy options is a critical first step. It equips you to have a truly informed discussion with your doctor, because finding the right delivery method can make all the difference in achieving consistent, life-changing results.
Weighing The Benefits, Risks, And Side Effects

Every medical therapy is a balancing act between potential gains and known risks. Understanding this is central to seeing the real difference between HRT and TRT. Because each therapy targets different hormones and patient profiles, you can't just lump their benefits and side effects together. A nuanced look is far more useful than a simple pros-and-cons list.
What HRT Can Offer (And Its Cautions)
Hormone Replacement Therapy is probably best known for bringing significant relief from disruptive menopausal symptoms. By restoring estrogen and progesterone, HRT can effectively dial down hot flashes, improve sleep quality, and stabilize mood swings that can feel completely overwhelming.
It also plays a crucial long-term role in helping maintain bone density, which is a major factor in reducing the risk of osteoporosis in postmenopausal women.
However, HRT isn't without potential risks. Historically, there have been concerns about an increased risk of blood clots and certain types of cancer. Modern medicine has gotten much smarter about this. Today's protocols mitigate these risks through careful patient screening, using the lowest effective dose, and often preferring transdermal (skin) applications over oral pills, which are easier on the liver.
TRT Benefits And Potential Downsides
Testosterone Replacement Therapy delivers a completely different set of outcomes, tailored specifically for men diagnosed with hypogonadism. The primary benefits often include a noticeable surge in energy levels, a restored libido, and an enhanced ability to build and maintain muscle mass. Many men also report a better mood, sharper mental clarity, and an overall greater sense of vitality.
The potential risks tied to TRT are specific to what it does: increase testosterone. One key concern is polycythemia, a condition where the body overproduces red blood cells, which can thicken the blood and potentially increase clot risk. Other considerations include acne, oily skin, and the need for ongoing monitoring of prostate health, as testosterone can worsen existing prostate conditions.
You can get a much deeper look into these factors by exploring the specific TRT benefits and risks in our dedicated guide.
The crucial takeaway is that neither therapy is inherently "safe" or "dangerous." Safety is achieved through a partnership with a qualified clinician who customizes the protocol, uses proper screening, and performs continuous monitoring to manage potential side effects before they become serious problems.
Ultimately, whether we're talking about HRT or TRT, the goal is always to make sure the benefits profoundly outweigh the risks. This is accomplished through personalized medicine, where regular lab testing and open communication with your doctor allow for adjustments that keep the therapy both effective and safe for the long haul.
How to Choose the Right Therapy for You
Deciding between HRT and TRT isn't a choice you should ever make on your own. The single most important step you can take is to work with a qualified medical professional who truly understands the nuanced differences between them and can guide you toward a protocol that is both safe and effective.
This entire journey starts with data. Your doctor will order a comprehensive panel of lab tests to get a complete picture of your hormone levels, including testosterone, estrogen, and other key markers. This isn't just a simple blood draw; think of it as a detailed hormonal blueprint that provides the objective evidence needed for a proper diagnosis.
Starting the Conversation with Your Doctor
Once your lab results are in, the next step is a deep dive into your symptoms and medical history. This is where your personal experience meets the clinical data, and a good clinician will listen intently to what you're feeling day-to-day.
To see how this plays out, let's look at two common scenarios:
- Case Study 1: A Woman in Menopause. A 52-year-old woman is struggling with severe hot flashes, night sweats, and mood swings that are disrupting her life. Her lab work comes back confirming low estrogen and progesterone. For her, a comprehensive HRT protocol designed to restore these specific hormones is the logical path forward.
- Case Study 2: A Man with Fatigue. A 45-year-old man reports feeling chronically tired, with a low libido and difficulty maintaining muscle mass despite regular workouts. His blood tests reveal testosterone levels well below the optimal range. In his case, a targeted TRT program is the appropriate solution.
These examples show exactly how symptoms and lab results work together to point to the right therapy. The treatment has to match the specific hormonal deficiency that's causing the problem.
Your personal health goals are a vital piece of the puzzle. Be crystal clear with your doctor about what you want to achieve—whether it’s more energy, better sleep, or a restored sex drive. This ensures the treatment plan is aligned with your desired outcomes.
As you navigate the world of online hormone clinics and telehealth providers, you need to be selective. Look for reputable clinics that insist on comprehensive lab work, offer personalized consultations with licensed physicians, and provide ongoing monitoring. Steer clear of any service pushing a one-size-fits-all solution, because personalized care is the absolute cornerstone of successful hormone therapy. Your health depends on a protocol designed specifically for you.
HRT And TRT: Your Questions Answered
Even with a clear understanding of the basics, some specific questions almost always come up. Let's tackle the most common ones to clear up any lingering confusion about how these therapies are used in the real world.
Can A Woman Use TRT Instead Of HRT?
Not exactly. While TRT is a male-focused therapy, a woman can be prescribed testosterone, but it's almost always part of a broader HRT plan. If a woman shows clear clinical signs of testosterone deficiency—like persistent fatigue or a tanked libido that doesn't improve with estrogen—a small, carefully managed dose might be added to her protocol.
It's almost never used as a standalone therapy for women the way it is for men. The dosage is also significantly lower to avoid any masculinizing side effects.
Can A Man Use HRT Instead Of TRT?
Yes, and this is a scenario we see quite often. While TRT is the go-to for low testosterone, some men, particularly as they get older, find that their issues go beyond just T levels. They might also have declining DHEA or sluggish thyroid hormones.
In this situation, a more comprehensive HRT approach is the smarter move. It's often called "hormone optimization" because the strategy shifts from fixing one number to balancing the entire hormonal picture for complete wellness.
The bottom line is this: the therapy has to match the diagnosed deficiency. Whether it's HRT or TRT, the decision is always driven by detailed lab work and a thorough review of your symptoms with a qualified medical professional. This ensures your treatment is both effective and safe.
Ready to explore a personalized approach to hormone optimization? Elite Bioscience offers tailored therapies designed to help you regain your vitality. With our expert medical guidance and discreet, at-home delivery, taking control of your health has never been easier. Learn more and start your journey at https://elitebioscience.co.